In a groundbreaking study recently published in Translational Psychiatry, researchers have unveiled compelling evidence that dysfunction in GABAergic interneurons plays a pivotal role in the aberrant neural network oscillations associated with epileptiform activity in PPT1-deficient mice. This discovery illuminates new pathways for understanding the mechanisms underpinning epilepsy and offers promising avenues for therapeutic development aimed at restoring neural circuit stability in affected individuals.
Neural oscillations—the rhythmic electrical activity generated by neuronal ensembles—serve as the fundamental basis for brain function, underpinning processes such as cognition, memory, and sensory perception. The delicate balance between excitation and inhibition within the neural circuitry is essential for maintaining these oscillations. Central to this balance are GABAergic interneurons, a specialized class of inhibitory neurons responsible for modulating excitatory signals to prevent excessive neuronal firing. Disruption in these interneurons, as implicated by the current study, foments a chaos in neural rhythms that manifest as epileptiform discharges.
The research team, led by Tong, J., Liu, W., and Wang, Q., harnessed a robust animal model: PPT1-deficient mice, which lack the palmitoyl-protein thioesterase 1 enzyme vital for normal neuronal function. These mice exhibit phenotypes mimicking human neuronal ceroid lipofuscinoses, a group of neurodegenerative disorders. By capitalizing on this model, the scientists could meticulously dissect the cellular and network-level abnormalities emerging from PPT1 deficiency.
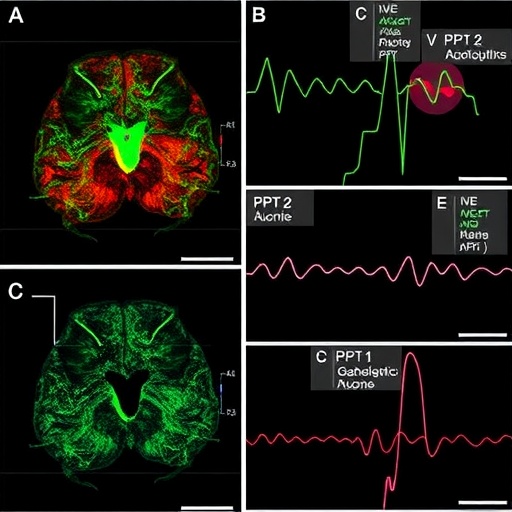
Advanced electrophysiological recordings revealed stark alterations in the oscillatory patterns within the hippocampus, a brain region integral to memory formation and a common site for epileptic focus. Specifically, the researchers observed diminished gamma oscillations—high-frequency rhythms crucial for synaptic plasticity and information encoding. These oscillatory disruptions were temporally correlated with spontaneous epileptiform events, suggesting a causative linkage mediated by impaired inhibitory control.
The mechanistic roots of these disturbances appeared concentrated on GABAergic interneurons. Through a combination of immunohistochemistry and in vitro patch-clamp techniques, the authors demonstrated a pronounced decrease in the excitability and synaptic output of parvalbumin-positive interneurons in the PPT1-deficient mice. These interneurons, known for their role in generating gamma oscillations, exhibited reduced expression of key proteins involved in GABA synthesis and release, culminating in weakened inhibitory signaling.
Intriguingly, the study also identified structural deficits within synapses, including diminished synaptic vesicle recycling and altered postsynaptic responsiveness. These findings point towards a multifaceted impairment encompassing not just the electrophysiological capacity of interneurons but also their molecular and synaptic integrity. This comprehensive breakdown culminates in an excitatory-inhibitory imbalance, tipping the scales toward hyperexcitability and epileptiform pathophysiology.
Among the more novel aspects of the research was the exploration of network-level consequences through computational modeling. By integrating their empirical data into biologically realistic neural network simulations, the researchers recapitulated the oscillatory fragmentation and epileptiform bursts observed in vivo. These models underscored the sufficiency of GABAergic interneuron dysfunction to induce pathological oscillatory patterns, thus cementing their centrality in the disease mechanism.
From a translational perspective, the study’s insights spotlight GABAergic interneurons as a promising therapeutic target. Current antiepileptic drugs largely focus on dampening overall neuronal excitability, often accompanied by broad central nervous system side effects. The potential to selectively restore or enhance interneuron function opens the door to more precise and effective interventions, mitigating seizures by rebalancing inhibitory circuits rather than suppressing neuronal activity indiscriminately.
Moreover, these findings bear implications beyond epilepsy. The intricate interplay of inhibitory interneurons in shaping neural oscillations is fundamental across myriad neuropsychiatric disorders, including schizophrenia and autism spectrum disorders. Hence, unraveling the molecular underpinnings of interneuron dysfunction in PPT1 deficiency may provide a foundational framework applicable to a spectrum of neurological conditions marked by disrupted neural rhythms.
The authors also emphasize the importance of early intervention, given that the synaptic and network abnormalities manifest progressively in PPT1-deficient mice. This timeline suggests a therapeutic window during which restoring GABAergic function could potentially halt or reverse the trajectory of epileptiform activity and associated cognitive deficits, highlighting the need for biomarkers that can detect interneuron dysfunction at prodromal stages.
Further research remains essential to delineate whether similar mechanisms underlie epilepsy in human patients with PPT1 mutations or related neurodegenerative diseases. While the animal model presents a compelling parallel, clinical validation through electrophysiological studies and molecular profiling will be critical. Future investigations may also explore gene therapy or pharmacological agents aimed at boosting palmitoyl-protein thioesterase 1 activity or directly enhancing GABAergic interneuron viability and function.
In conclusion, this seminal work by Tong and colleagues powerfully underscores the intertwined relationship between molecular enzyme deficiencies, interneuronal dysfunction, and aberrant neural oscillations leading to epileptiform phenomena. By shedding light on the cellular culprits and network consequences of PPT1 deficiency, the study marks a transformative step in epilepsy research, steering the field towards targeted neuromodulatory therapies that promise improved efficacy and fewer side effects.
As the neuroscience community digests these findings, the quest to translate such knowledge into clinical breakthroughs intensifies. Harnessing the potential of GABAergic interneurons to orchestrate balanced neural activity offers hope not only for individuals suffering from epilepsy but also for advancing our fundamental understanding of brain circuitry and its vulnerabilities.
The study’s synergy of electrophysiology, molecular biology, and computational modeling exemplifies the multidisciplinary approach needed to unravel the brain’s complexity. It is a vivid reminder that even subtle disruptions at the cellular level can ripple outward, instigating profound changes in brain function and behavior. Through endeavors such as this, the path toward conquering neurological disorders becomes progressively clearer.
Subject of Research: Dysfunction of GABAergic interneurons leading to altered neural oscillations associated with epileptiform activity in PPT1-deficient mice.
Article Title: Dysfunction of GABAergic interneurons underlies altered neural network oscillations associated with epileptiform activity in PPT1-deficient mice.
Article References:
Tong, J., Liu, W., Wang, Q. et al. Dysfunction of GABAergic interneurons underlies altered neural network oscillations associated with epileptiform activity in PPT1-deficient mice. Transl Psychiatry (2026). https://doi.org/10.1038/s41398-026-03843-8
Image Credits: AI Generated