In a groundbreaking new study published in JAMA Network Open, researchers have identified a concerning correlation between the use of cutting-edge diabetes medications and rare but serious optic nerve disorders. This meticulously conducted investigation focused on patients with type 2 diabetes who had no documented prior ophthalmic conditions, shedding light on the nuanced relationship between therapeutic advances and unforeseen neurological complications. Semaglutide and tirzepatide, two innovative injectable therapies hailed for their efficacy in glycemic control and weight management, were linked to an increased risk of nonarteritic anterior ischemic optic neuropathy (NAION) and other optic nerve pathologies, albeit with an overall low incidence.
Type 2 diabetes mellitus (T2DM) remains a global health challenge marked by chronic hyperglycemia and an escalating prevalence, fueling intense research into novel pharmacologic interventions. Semaglutide, a glucagon-like peptide-1 receptor agonist (GLP-1 RA), and tirzepatide, a recent dual glucose-dependent insulinotropic polypeptide and GLP-1 receptor agonist, represent therapeutic milestones accelerating glycemic regulation while conferring cardiovascular benefits. However, the study’s findings underscore the critical need to balance these metabolic advantages against potential adverse neurological effects, particularly within the delicate microvascular architecture of the optic nerve head.
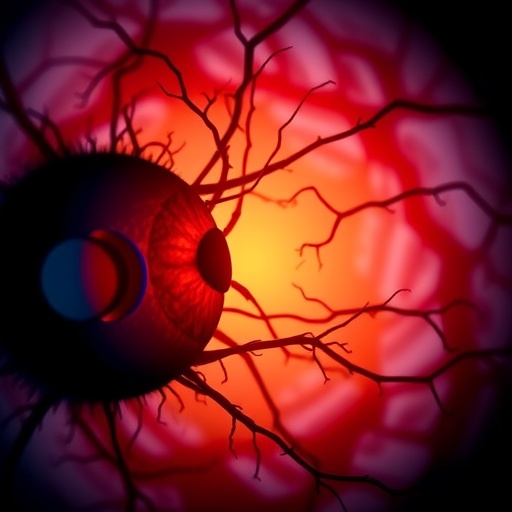
Delving into the mechanistic pathways, the optic nerve is exceptionally vulnerable to ischemic insults due to its unique circulation, reliant on short posterior ciliary arteries without significant collateral flow. In NAION, diminished perfusion results in sudden vision loss, often accompanied by optic disc swelling. The researchers postulate that semaglutide and tirzepatide may exacerbate underlying microvascular insufficiency or provoke inflammatory cascades, contributing to optic nerve ischemia. Although causality remains to be definitively established, the temporal association and biological plausibility warrant heightened clinical vigilance.
This investigation leveraged extensive patient data, utilizing rigorous epidemiological methods and advanced statistical modeling to adjust for confounders such as age, glycemic control, and baseline cardiovascular risk. The patient cohort was carefully curated to exclude prior eye conditions, ensuring an unbiased assessment of incident optic neuropathies. Data revealed a statistically significant but quantitatively modest elevation in the incidence of NAION among those treated with these agents compared to other antidiabetic drugs, highlighting a rare but meaningful safety signal.
Crucially, the overall risk remains low, and the substantial benefits of semaglutide and tirzepatide in managing complex metabolic profiles are undisputed. Clinicians are advised to maintain a cautious approach, incorporating comprehensive ophthalmological evaluations at baseline and during therapy, especially for patients with predisposing risk factors such as nocturnal hypotension or crowded optic discs. Patient education on recognizing sudden vision changes can prompt timely intervention, potentially mitigating irreversible visual sequelae.
The findings stimulate important questions for future research, including elucidation of the molecular underpinnings governing GLP-1 RA-related optic nerve vulnerability. It is imperative to decipher whether these effects are idiosyncratic or dose-dependent and to investigate potential protective strategies. Moreover, longer follow-up studies are essential to characterize the trajectory of optic nerve health over prolonged therapy, particularly given the chronic nature of T2DM treatment.
From a pharmacovigilance perspective, this study exemplifies the evolving paradigm where innovative therapies necessitate ongoing, meticulous safety monitoring. As the armamentarium against diabetes expands with biotechnological advances, uncovering rare adverse events ensures that patient safety remains paramount. Regulatory agencies and healthcare providers must collaborate closely, refining prescribing guidelines and surveillance protocols accordingly.
The clinical community is also encouraged to integrate multidisciplinary perspectives, elevating the role of ophthalmologists in diabetes care teams. Enhanced screening protocols, leveraging emerging imaging modalities like optical coherence tomography angiography, can enable earlier detection of subclinical optic nerve changes. This proactive stance may transform outcomes, preserving vision while optimizing metabolic health.
While the study focused predominantly on NAION, other optic nerve disorders were also noted, suggesting a broader spectrum of possible neuro-ophthalmic complications linked with these drugs. This highlights the necessity to remain alert to diverse ocular pathologies and fosters an expanded understanding of diabetes-related neurological risk factors in the era of novel drug classes.
In summary, the remarkable therapeutic efficacy of semaglutide and tirzepatide is tempered by a rare but notable association with optic nerve ischemic events. This dual-edge reality encapsulates the complexities innate in modern medicine, where breakthroughs carry nuanced risks. Stakeholders across research, clinical practice, and patient advocacy must synergize efforts to optimize therapeutic algorithms, ensuring maximal benefit while minimizing harm.
This study, led by Rong Xu, PhD, represents a pivotal contribution to diabetes pharmacotherapy safety literature. The call for vigilant patient monitoring and continued investigative rigor sets a new standard in balancing innovation and caution. As the field advances, these insights will guide clinicians in delivering tailored, informed care to millions grappling with type 2 diabetes worldwide.
Subject of Research:
Type 2 diabetes treatment-related optic nerve disorder risks
Article Title:
Not specified in the provided content
News Publication Date:
Not specified in the provided content
Web References:
doi:10.1001/jamanetworkopen.2025.26327
References:
Not specified in the provided content
Image Credits:
Not specified in the provided content
Keywords
Optics; Nerve injuries; Medications; Type 2 diabetes; Medical treatments; Vision disorders; Risk factors; Patient monitoring