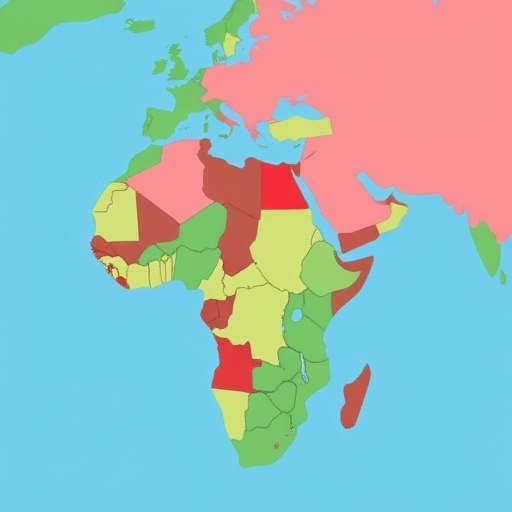
In a groundbreaking qualitative study that traverses the vibrant and diverse landscapes of Africa, researchers have unearthed critical insights into the operations of health professions education units across Eastern, Southern, and Western regions of the continent. This rigorous investigation, led by an esteemed consortium of scholars including Welch, Hansen, and Nawagi, sheds light on the multifaceted functions, prevailing challenges, and promising opportunities that these educational institutions offer in a rapidly evolving healthcare landscape. The study comes at a pivotal time, as Africa grapples with increasing health demands compounded by a myriad of socio-economic factors and public health crises.
The diverse educational units under scrutiny are pivotal in shaping the healthcare workforce, yet the study reveals that they often operate in an environment riddled with challenges. These include resource scarcity, infrastructural deficits, and the critical need for curriculum adaptation to meet both local and global health needs. The researchers undertook a comprehensive qualitative methodology, which included interviews, focus groups, and surveys to capture a wide range of perspectives from educators, students, and healthcare practitioners. The robust data collection process ensures that the findings are reflective of the realities on the ground in varied African contexts.
One of the foremost insights from the research indicates a pressing need for innovative teaching methodologies tailored to the unique health challenges faced in different regions. As health threats evolve—ranging from communicable diseases to emerging public health crises—the educational strategies employed in training health professionals must keep pace. This is particularly crucial in rural areas, where access to medical education is limited and where a new generation of health workers is urgently needed. The study underscores a gap between existing educational frameworks and the practical realities of healthcare delivery in Africa, suggesting that a paradigm shift towards more adaptive learning structures is essential.
Furthermore, the research highlights the often-overlooked role of technology in enhancing medical education. The proliferation of digital tools and platforms presents an untapped potential for expanding access to quality educational resources. While some educational institutions have begun experimenting with hybrid learning models, many remain hesitant to fully embrace digital methodologies, primarily due to concerns over equity and access. The researchers argue that with the right support and infrastructure, technology could serve as a great equalizer, bridging the educational gap between urban and rural populations and fostering a more robust healthcare workforce.
Another prevailing theme in the findings is the imperative of fostering regional collaborations among health professions education units. The importance of sharing best practices, resources, and research across borders cannot be overstated. The study advocates for a more integrated approach to health education that transcends regional divides, allowing institutions to pool resources and expertise. Such collaboration may also lead to innovations in curriculum development, research, and even policy-making, addressing the collective challenges faced by the region more effectively.
The challenges identified in the study are not merely logistical; they are also deeply cultural. The authors note that many health professions education units grapple with ingrained attitudes towards healthcare practices that may not align with modern pedagogical frameworks. Resistance to change, whether due to tradition or a lack of awareness of new methodologies, often hinders progress. The researchers emphasize the need for a cultural shift that embraces a continuous learning ethos among educators and students alike. Such a transformation is essential not only for improving educational outcomes but also for ensuring that health professionals are equipped to meet the diverse needs of their communities.
The opportunities for advancement in health professions education in Africa are vast, and they extend well beyond the confines of traditional education. Notably, the study draws attention to the potential for interdisciplinary education models that combine health training with skills from other sectors, such as communication, technology, and community engagement. This holistic approach could facilitate the development of well-rounded professionals capable of tackling the complex health challenges of the 21st century. By promoting such interdisciplinary collaborations, educational units can cultivate a workforce that is responsive to the dynamics of health delivery in varied cultural contexts.
As the researchers delve deeper into the narratives collected, there is a discernible call for policy interventions that support the growth and sustainability of health professions education units. This includes advocating for increased funding, better infrastructural support, and greater recognition of the vital role that these educational institutions play in public health. The findings suggest that policymakers should prioritize educational reforms that empower institutions to respond meaningfully to both global health trends and local health needs.
Importantly, the influence of international partnerships on the development of health education cannot be ignored. The study finds that such collaborations often lead to valuable exchanges of knowledge and resources, enhancing the capacity of local institutions. However, there is caution against dependency on external funding or curricula that may not align with local realities. The researchers argue for a balanced approach that draws on global expertise while remaining firmly rooted in the local context.
In light of the evolving healthcare landscape, the researchers advocate for continuous assessment and adaptation of educational programs. What works today may not suffice tomorrow; therefore, regular evaluations of curricula and teaching methodologies are crucial to ensuring that health professionals are adequately prepared for future challenges. This iterative process not only fosters accountability but also encourages innovation within educational institutions.
Moreover, the startling disparities in health outcomes across African nations necessitate urgent attention to the equity of educational opportunities. The authors highlight the importance of targeted initiatives aimed at underrepresented groups to ensure that the future workforce reflects the diversity of the populations it serves. Providing equitable access to quality education for all, regardless of socio-economic status or geographical location, is paramount for building a resilient healthcare system.
As this qualitative study illustrates, the functions of health professions education units in Africa extend far beyond traditional educational roles. They are pivotal in shaping the future of health care delivery, responding to local and global health issues, and fostering a culture of collaborative learning and continuous improvement. As the continent grapples with pressing health challenges, reforms and innovations within these educational institutions will be critical for enabling a new generation of health professionals to thrive.
In conclusion, the findings of this study open a dialogue on the present state and future potential of health professions education in Africa. As highlighted throughout the research, there exists a significant opportunity for transformation within these educational units if they can harness the collaborative spirit of the continent’s diverse healthcare communities. The forthcoming years will undoubtedly be crucial as these institutions seek to capitalize on their strengths, address existing challenges, and ultimately fulfill their vital roles in fostering health equity across the African region.
Subject of Research: Functions, challenges and opportunities of health professions education units in Africa
Article Title: Functions, challenges and opportunities of health professions education units in Africa: a qualitative study across Eastern, Southern and Western regions.
Article References: Welch, S.B., Hansen, A., Nawagi, F. et al. Functions, challenges and opportunities of health professions education units in Africa: a qualitative study across Eastern, Southern and Western regions. BMC Med Educ (2026). https://doi.org/10.1186/s12909-025-08403-0
Image Credits: AI Generated
DOI: 10.1186/s12909-025-08403-0
Keywords: health professions education, Africa, qualitative study, healthcare workforce, challenges, opportunities, interdisciplinary education, policy interventions, equity, technological advancement.