In recent years, the field of microsurgery has seen unprecedented growth, driven largely by advances in surgical techniques, technology, and training methodologies. A pivotal study led by researchers Tsiklin, Jacobs, and Verhelst emphasizes an essential aspect of this progress: the optimization of non-living animal models for simulation-based microsurgical training. The findings, published in BMC Medical Education, shed light on the critical need for innovative training tools that can enhance the skills of surgeons without the ethical and logistical complications associated with live animal models.
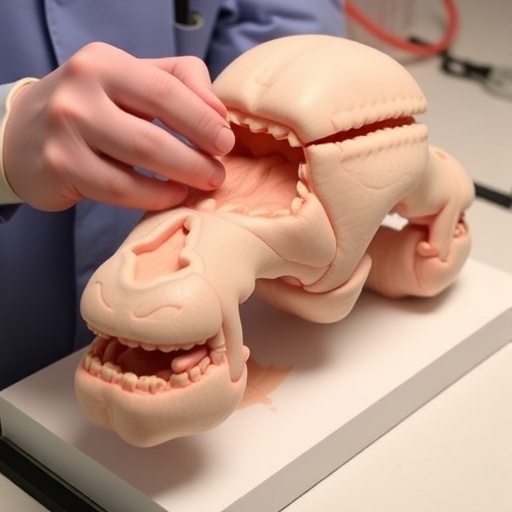
The use of non-living animal models is revolutionizing how microsurgeons are trained. Traditional training methods have often relied on live animal surgeries, which can be ethically challenging and may not provide the best learning experiences for trainees. The study explores alternative approaches, demonstrating that high-fidelity simulation models can offer a more effective and ethical solution. By optimizing these non-living models, the researchers aim to create a training environment that closely mimics real-life surgical scenarios while being devoid of the ethical implications that come with using live animals.
One of the key advantages of utilizing non-living models in surgical training is the ability to repeat procedures without the fear of harming sentient beings. The study finds that these models can be manipulated and reused, allowing for multiple training sessions for different surgical scenarios. Trainees can practice suturing, anastomosis, and other delicate surgical techniques in a controlled environment that closely simulates real-life conditions. This gives them the opportunity to hone their skills until they achieve a level of proficiency that can translate into actual surgeries.
The researchers employed various measurement techniques to evaluate the effectiveness of the non-living models they developed. They assessed metrics such as precision, speed, and learning curve improvements, which are crucial for microsurgical tasks. Their results demonstrated that trainees utilizing optimized non-living models showed a significant improvement in skill acquisition compared to those trained with traditional methods. This empirical evidence strengthens the case for transitioning towards more ethical and effective training modalities in surgical education.
In addition to enhancing surgical skills, the study also highlights how simulation-based training using non-living models can impact the psychological preparedness of trainees. Surgical training often comes with a significant amount of stress and anxiety, particularly in high-stakes environments. The repeated practice allowed by using non-living models can help trainees build confidence in their abilities, thereby improving their overall performance when they eventually perform procedures on live patients.
The implications of these findings extend beyond individual surgical training. By adopting non-living animal models, medical institutions can address larger ethical concerns about the use of live subjects in training programs. The advancements in simulation technologies not only promote skill development but also align with the growing demand for more humane and ethical education practices in the medical field.
Moreover, the study discusses the potential for these non-living models to be tailored for various surgical specialties beyond microsurgery. As medical education continues to evolve, the cross-disciplinary applications of simulation training become increasingly apparent. The techniques uncovered in this research could be adapted for use in orthopedics, cardiovascular surgery, and more, creating a new standard in how future surgeons across different specialties are trained.
Importantly, this research could influence policy changes regarding surgical training programs worldwide. If more institutions adopt simulation-based training using optimized non-living models, it could lead to widespread reforms in how medical education is conducted. This would not only enhance the skill set of upcoming surgeons but also promote a culture of ethical responsibility within the medical community, prioritizing patient safety and welfare above all.
The study’s findings also open doors to interdisciplinary collaborations between educators, surgeons, and technology developers. As the medical field continues to integrate technology into standard training practices, the development of more sophisticated simulation models can benefit from input across various domains. Experts in virtual reality, biomechanics, and educational psychology can contribute to creating even more effective training solutions that are reflective of real-life challenges faced in the operating room.
In conclusion, the optimization of non-living animal models for simulation-based microsurgical training is a groundbreaking advancement that promises to reshape surgical education. As these models are refined and adopted, future generations of surgeons will have access to better training tools, resulting in improved surgical outcomes and heightened patient safety. The study led by Tsiklin and his colleagues paves the way for a more ethical and effective approach to medical training that resonates with the values of the modern healthcare landscape.
The shift to simulation-based training utilizing non-living models is an example of how innovation can address longstanding ethical dilemmas in medicine. As the impact of this research unfolds, we may witness a transformation not only in surgical training but throughout the broader context of medical education. This progress will play a crucial role in the evolution of healthcare, ensuring that training aligns with contemporary values while producing highly skilled professionals prepared to tackle the complexities of modern medicine.
Embracing the potential of non-living models in surgical training could position healthcare institutions at the forefront of educational excellence. By fostering a culture of innovation and commitment to ethical standards, these institutions can inspire a new generation of healthcare providers who are equipped with the necessary skills and confidence to improve patient outcomes across the globe.
As we reflect on these developments, it is imperative that stakeholders remain engaged in ongoing dialogue about the future of surgical education and the ethical responsibilities that come with it. The research by Tsiklin and colleagues provides a foundation for this discourse, highlighting the vital role of simulation in shaping the future of healthcare.
Subject of Research: Optimization of non-living animal models for simulation-based microsurgical training.
Article Title: Optimization of the non-living animal models for simulation-based microsurgical training.
Article References: Tsiklin, I., Jacobs, R., Verhelst, PJ. et al. Optimization of the non-living animal models for simulation-based microsurgical training. BMC Med Educ 25, 1510 (2025). https://doi.org/10.1186/s12909-025-07979-x
Image Credits: AI Generated
DOI: 10.1186/s12909-025-07979-x
Keywords: microsurgery, simulation-based training, non-living animal models, surgical education, ethical practice, skill acquisition, technological advancements, healthcare training.