A recent cohort study has illuminated significant disparities in the fulfillment of prescriptions for glucagon-like peptide-1 receptor agonists (GLP-1RAs), a class of medications pivotal in managing type 2 diabetes and obesity. The study revealed a notable 40% of orders for these medications were never filled, underscoring critical gaps in medication adherence that could profoundly influence health outcomes. This omission is particularly alarming given the proven efficacy of GLP-1RAs in glycemic control and weight reduction, which are essential components of comprehensive diabetes care.
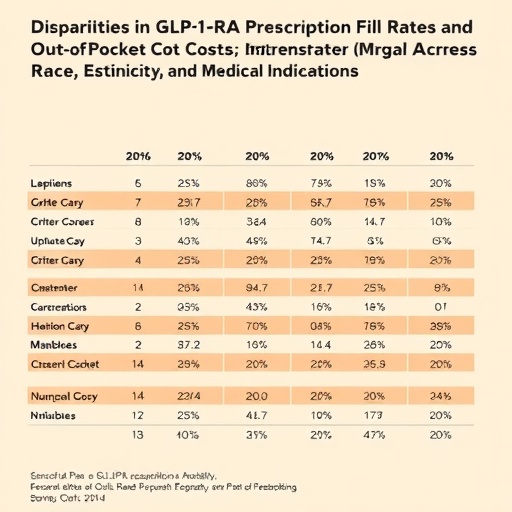
The study delved deeper into demographic variations, uncovering that non-Hispanic Black and Hispanic patients were statistically less likely to fill their GLP-1RA prescriptions than their non-Hispanic white counterparts. This discrepancy highlights persistent racial and ethnic inequities in access to crucial pharmaceuticals, raising concerns about systemic barriers that may hinder equitable healthcare delivery. Understanding the nuances of these disparities is imperative not only for clinicians but also for policymakers aiming to bridge gaps in chronic disease management.
Financial factors emerged as a complex contributor to these disparities. Intriguingly, among those who did manage to fill their prescriptions, non-Hispanic Black and Hispanic patients incurred lower out-of-pocket costs compared to non-Hispanic white patients. This counterintuitive finding suggests that cost alone does not fully explain the differences in medication fulfillment. Instead, it points to a confluence of insurance coverage variability, possible differential prescribing patterns concerning specific GLP-1RA agents, and divergent thresholds of cost acceptability that influence patients’ decisions to adhere to prescribed regimens.
Insurance coverage intricacies likely play a pivotal role in shaping these outcomes. Variations in formularies, drug tier placements, copay structures, and prior authorization requirements can markedly impact patients’ ability and willingness to obtain prescribed medications. Minority populations often face disproportionate challenges in insurance stability and coverage adequacy, which may translate into higher barriers to filling prescriptions despite potential financial assistance or discounts available to some groups.
Pharmacological nuances of different GLP-1RA agents might also contribute to out-of-pocket cost differences. The class encompasses multiple drugs varying in molecular structure, dosing frequencies, administration routes, and market prices. Prescribing patterns influenced by provider preference, patient characteristics, or formulary restrictions could lead to differential exposure to more or less expensive agents among racial and ethnic groups, indirectly affecting the likelihood of prescription fulfillment.
The divergent economic thresholds for medication adherence identified in this study invite further exploration into socio-cultural and psychological dimensions influencing patient behavior. Perceived value, health literacy, trust in medical interventions, and prior experiences with the healthcare system might all factor into decisions surrounding medication procurement. Such factors are often intertwined with broader social determinants of health that disproportionately affect minority communities.
This research, published in an international peer-reviewed journal dedicated to health policy and healthcare strategy, underscores the complexity of medication adherence beyond purely clinical considerations. It advocates for a multidisciplinary approach encompassing economic, social, and systemic interventions aimed at enhancing equitable access to life-altering therapies like GLP-1RAs. Addressing these disparities could substantially mitigate the burden of diabetes-related complications among underserved populations.
The findings resonate with a growing body of literature emphasizing racial and ethnic disparities in chronic disease management. They contribute novel insights into how cost dynamics and insurance mechanisms mediate access inequities. Such evidence is critical for informing targeted policy reforms, including insurance redesign, subsidy programs, and culturally tailored patient education initiatives that could empower patients to overcome barriers to optimal treatment adherence.
Future research directions inspired by this study may involve granular analyses of insurance plan designs, qualitative investigations into patient and provider perspectives on GLP-1RA use, and randomized interventions testing strategies to increase prescription fulfillment among minority groups. Importantly, translational efforts bridging research findings to clinical practice and health policy will be pivotal in realizing tangible improvements.
In sum, this cohort study spotlights the multifactorial and intertwined determinants of GLP-1RA prescription fulfillment, revealing profound racial and ethnic disparities embedded within the US healthcare landscape. Its revelations challenge stakeholders to innovate and collaborate across sectors to ensure that progress in pharmaceutical development translates into equitable health benefits for all populations grappling with diabetes and obesity.
The study’s corresponding author, Dr. Ameet Sarpatwari, a scholar at the intersection of epidemiology, law, and public health, emphasizes the urgency of unpacking these disparities to catalyze systemic change. Interested readers and media representatives are encouraged to contact Dr. Sarpatwari directly for further details and access to the comprehensive study findings.
As the healthcare community continues to grapple with the complexities of chronic disease management in diverse populations, the insights from this investigation serve as a clarion call. They underscore that the promise of advanced pharmacotherapies can only be fulfilled when access barriers—financial, systemic, and psychosocial—are comprehensively addressed in contexts acknowledging and respecting racial and ethnic diversity.
Subject of Research: Racial and ethnic disparities in the fulfillment of glucagon-like peptide-1 receptor agonist prescriptions in a diverse patient population.
Article Title: [Not specified in the provided content]
News Publication Date: [Not specified in the provided content]
Web References: doi:10.1001/jamahealthforum.2025.4258
Keywords: Peptides, Agonists, Cohort studies, Racial differences, Ethnicity, Medications, Pharmaceuticals, Health care costs, Health insurance