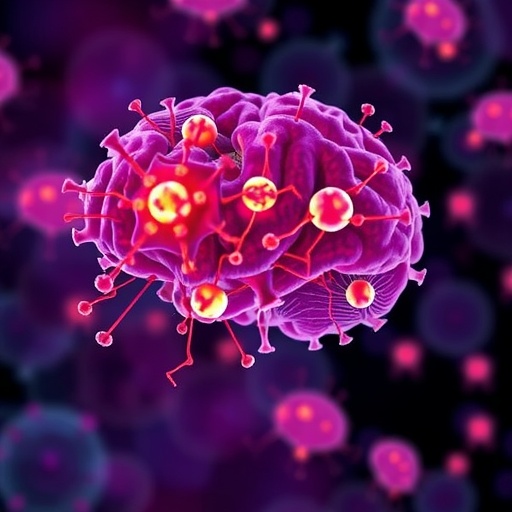
Recent studies have increasingly highlighted the intricate relationship between mental health and neuroinflammation, leading to new insights into the cognitive impairments observed in various psychiatric conditions. A groundbreaking paper by Lee et al. explores this relationship further by focusing on the effects of proinflammatory cytokines and programmed cell death on cognitive functioning in older adults diagnosed with bipolar disorder. As the understanding of these complex interactions deepens, it opens up new avenues for potential therapeutic interventions that could alleviate cognitive deficits in a population that is often overlooked in psychiatric research.
Bipolar disorder is a severe mental health condition characterized by extreme mood swings, ranging from manic episodes to depressive states. While the emotional and behavioral symptoms are often the focus of treatment, there is a growing recognition that cognitive symptoms can have a profound impact on the lives of those affected. Older adults with bipolar disorder frequently report difficulties with memory, attention, and problem-solving, significantly limiting their quality of life. In this study published in “Annals of General Psychiatry,” the authors delve into how biological factors, particularly inflammation, contribute to these cognitive deficits.
Cytokines, small proteins released by cells that have a specific effect on cell communication and behavior, play a pivotal role in the immune response. In cases of chronic inflammation, the levels of proinflammatory cytokines are elevated, leading to detrimental effects on the brain. Lee et al. present compelling evidence that older adults with bipolar disorder exhibit increased levels of these cytokines, which correspondingly correlate with cognitive impairment. This finding aligns with a wider body of literature suggesting that neuroinflammation may contribute to the pathophysiology of various neurodegenerative diseases.
The study employs a robust methodological framework, utilizing neuropsychological assessments alongside biomarker analyses to paint a comprehensive picture of cognitive function in the context of bipolar disorder. The researchers emphasize the importance of distinguishing between different cognitive domains, as deficits may not be uniform across the board. For example, while some individuals may struggle significantly with episodic memory, others might find their executive functions to be most severely impacted. This nuance is essential for tailoring interventions that address specific cognitive deficits rather than treating the disorder solely as a monolith.
A significant aspect of the research is the exploration of programmed cell death, or apoptosis, which is a natural process of cellular turnover. However, when dysregulated, apoptosis can lead to neurodegeneration. Lee et al. posit that elevated cytokine levels may accelerate this process in the brains of older adults with bipolar disorder, contributing to cognitive decline. This insight not only sheds light on the mechanisms underlying cognitive dysfunction but also raises questions about the interplay between inflammation and neurodegeneration.
The implications of these findings extend beyond academia; they suggest that therapeutic strategies targeting inflammation might hold promise for improving cognitive outcomes in this vulnerable population. Current treatments for bipolar disorder predominantly focus on mood stabilization and do not adequately address cognitive impairment. However, the emerging evidence points to the potential benefit of anti-inflammatory agents as adjunct therapies. This paradigm shift could herald a new era in the management of bipolar disorder, emphasizing a more holistic approach to treatment that encompasses both emotional and cognitive health.
Moreover, the intersection of aging and bipolar disorder presents unique challenges, particularly as the prevalence of the condition may rise among an aging population. As adults live longer and face the myriad public health challenges associated with aging, it is critical to address the cognitive complications that may arise in conjunction with mental health disorders. This study serves as a clarion call for researchers and clinicians alike to prioritize cognitive health in older patients with bipolar disorder and consider innovative approaches to treatment.
The potential societal impact of improving cognitive function in this demographic cannot be overstated. Enhanced cognitive abilities allow for greater independence, increased engagement in social activities, and overall improved quality of life. Furthermore, addressing cognitive impairments could reduce the burden on caregivers and healthcare systems, leading to economic benefits alongside improved patient outcomes. As the research community continues to unravel the complexities of mental health, the findings of Lee et al. highlight not merely an academic inquiry but a vital pursuit that holds the potential for significant societal change.
Finally, while the research by Lee et al. is incredibly promising, it also underscores the need for further studies to corroborate these findings and explore the underlying biological mechanisms in greater depth. Longitudinal studies will be particularly valuable, as they can track changes over time and assess the long-term effects of inflammation and cognitive health. Only through continued research can we hope to fully understand the ramifications of neuroinflammation on mental health and develop effective interventions that address the needs of older adults living with bipolar disorder.
As mental health research advances, so too does the need for awareness and advocacy surrounding the unique challenges faced by older adults with bipolar disorder. This study not only contributes important knowledge to the field but also highlights the pressing need for action in mental health care policy, ensuring that this vulnerable population receives the attention and resources necessary to thrive. Ultimately, Lee et al. make a significant contribution to our understanding of how biological processes interact with cognitive function, paving the way for future innovations in mental health treatment.
Through this vital research, we are moving closer toward unlocking the mysterious relationship between inflammation, cognition, and bipolar disorder. As we bear witness to the growing body of evidence, it becomes evident that a multi-faceted approach to treatment is not only necessary but also achievable. The future of bipolar disorder management lies in recognizing and addressing the complexities of cognitive impairment alongside emotion regulation, promising a brighter tomorrow for those affected by this challenging condition.
The expanding field of neuroinflammation research promises to illuminate further pathways to health and healing, with non-invasive treatments that target these pathways offering hope where there was previously little. A better understanding of this interplay holds the key to advancing mental health care and reshaping the narratives surrounding mental illness for older adults, enabling them to navigate their golden years with the dignity and mental clarity they deserve.
In conclusion, Lee et al.’s research is a call to arms for stakeholders across healthcare, policy, and research to prioritize the cognitive health of older adults with bipolar disorder. The insights gleaned from this study not only lay the groundwork for future inquiries but also inspire action tailored to meet the nuanced needs of this demographic. Bridging the gap between mental health and neurobiology may offer one of the most promising avenues for enhancing the lives of individuals living with bipolar disorder and, ultimately, fostering a more equitable and informed approach to mental health care.
Subject of Research: The impact of proinflammatory cytokines and programmed cell death on cognitive functioning in older adults with bipolar disorder.
Article Title: Effects of proinflammatory cytokines and programmed cell death on cognitive domains in older age patients with bipolar disorder.
Article References:
Lee, PY., Chiu, C.C., Kuo, PH. et al. Effects of proinflammatory cytokines and programmed cell death on cognitive domains in older age patients with bipolar disorder.
Ann Gen Psychiatry 24, 48 (2025). https://doi.org/10.1186/s12991-025-00591-9
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12991-025-00591-9
Keywords: Neuroinflammation, Bipolar Disorder, Cognitive Impairment, Older Adults, Proinflammatory Cytokines, Apoptosis, Mental Health, Therapeutic Interventions.