In a recent compelling development within the realm of neurodegenerative disease research, an international team of scientists has addressed critical cortical microstructural abnormalities linked to dementia with Lewy bodies (DLB) and how these anomalies intersect with Alzheimer’s disease copathologies. This correction and refinement of earlier work elucidate profound insights into the overlapping pathological mechanisms that underlie these devastating disorders, offering promising avenues for diagnostic precision and therapeutic innovation.
Dementia with Lewy bodies is frequently overshadowed in public discourse despite being the second most prevalent form of progressive dementia after Alzheimer’s disease. Characterized by the accumulation of alpha-synuclein protein aggregates in cortical and subcortical brain regions, DLB manifests through complex clinical presentations including cognitive fluctuations, parkinsonism, visual hallucinations, and rapid eye movement sleep behavior disorder. The intricate neuropathological landscape complicates clinical diagnosis, often involving copathologies typical of Alzheimer’s disease such as amyloid-beta plaques and tau neurofibrillary tangles.
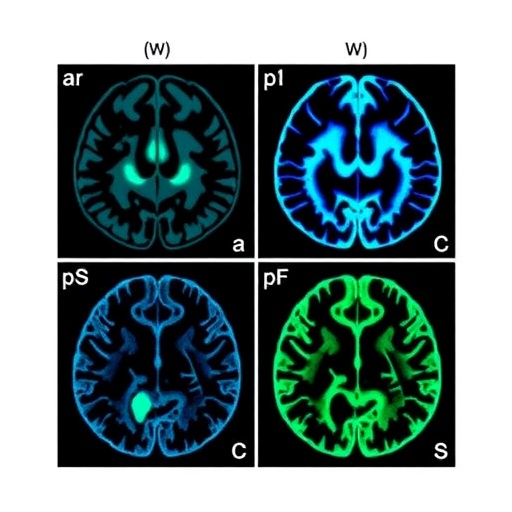
The research team, led by distinguished neuroscientists Mak, Reid, and Przybelski among others, revisited their previous findings to correct and expand upon the characterization of microstructural cortical abnormalities in DLB. Utilizing advanced neuroimaging modalities, including diffusion tensor imaging (DTI) and high-resolution magnetic resonance imaging (MRI), the study dissects microarchitectural changes in gray matter that are imperceptible to conventional neuroimaging techniques. These refined imaging approaches reveal pathological disruptions at the cellular and sub-cellular levels, encompassing axonal degradation, dendritic spine loss, and alterations in myelination.
One of the pivotal revelations of this study lies in the identification of specific microstructural signatures that correlate strongly with the degree of concomitant Alzheimer’s disease pathology within DLB patients. Through quantitative imaging metrics such as fractional anisotropy and mean diffusivity, researchers delineated patterns that differentiate pure synucleinopathies from mixed pathologies, thereby enhancing diagnostic accuracy. This differentiation is crucial as it has profound implications for treatment strategies, prognosis forecasting, and patient stratification in clinical trials.
Moreover, the study underscores the heterogeneity of dementia with Lewy bodies, emphasizing that the cortical microstructural landscape is not uniform across patients but varies in accordance with the extent and regional distribution of Alzheimer’s disease copathologies. Correlating these findings with postmortem histopathological analyses, the researchers confirm that amyloid and tau burdens intensify microstructural damage in neocortical regions traditionally implicated in cognitive and executive dysfunction.
The correction addressed in the publication also highlights methodological advancements in imaging protocols and data analysis pipelines. These improvements ensure more reliable biomarkers and reproducibility, which are vital for the translation of research into clinical practice. Precisely, the incorporation of multi-shell diffusion imaging and sophisticated machine learning algorithms enables a more granular understanding of white and gray matter interactions, a dynamic facet critically altered in mixed dementia pathologies.
Clinically, these insights shed light on why patients with DLB often experience a variable spectrum of symptom severity and disease progression. The overlap with Alzheimer’s copathologies not only complicates the clinical phenotype but potentially modulates responses to pharmacological interventions such as cholinesterase inhibitors and dopaminergic agents. Understanding the microstructural substrates can therefore inform personalized medicine approaches, guiding the selection of targeted therapies to optimize cognitive outcomes and quality of life.
The interrelation between alpha-synucleinopathy characteristic of DLB and amyloid-tau pathology hallmarking Alzheimer’s disease suggests underlying mechanistic synergies or pathogenic cascades. The research raises compelling questions regarding whether amyloid or tau deposition might exacerbate synuclein aggregation or vice versa, fueling a vicious cycle of neurodegeneration. These findings provoke further inquiry into the molecular crosstalk driving disease overlap and potential combinatorial therapeutic targets that may interrupt this pathological interplay.
From a technological standpoint, the utilization of cutting-edge neuroimaging technologies in this study sets a precedent for future neuropathological investigations. The integration of computational neuroscience, neuroinformatics, and advanced imaging creates a powerful framework capable of disentangling the microstructural complexities of mixed dementia syndromes. This multidisciplinary approach redefines our capacity to detect subtle brain alterations prior to overt cognitive decline, potentially catalyzing earlier diagnosis and intervention.
Importantly, this work extends beyond the lab to influence biomarker development for clinical trials and routine screening. Reliable, non-invasive biomarkers capable of distinguishing pure DLB from mixed pathology cases would revolutionize clinical workflow, aid prognosis assessment, and enable stratified enrollment for experimental therapeutics. The validation of these cortical microstructural markers enhances the robustness of neurodegenerative disease classification systems.
Ethically, the study’s results underline the necessity for transparent communication with patients and families regarding the complexities and uncertainties inherent in dementia diagnoses. Recognizing the interplay of multiple pathologies informs realistic expectations about disease trajectory and therapeutic efficacy, crucial factors in care planning. Meanwhile, the research community must grapple with the challenge of translating microstructural insights into accessible clinical tools understandable by healthcare providers and patients alike.
Looking ahead, the intersection between dementia with Lewy bodies and Alzheimer’s disease pathologies uncovered by this study prompts a paradigm shift in neurodegenerative disease conceptualization. Rather than viewing disorders as isolated entities, a spectrum model acknowledging overlapping mechanisms and phenotypic diversity emerges. This conceptual evolution necessitates novel research strategies that incorporate holistic views of brain pathology, bridging molecular, structural, and functional domains.
In summary, the author correction led by Mak and colleagues refines our comprehension of the subtle yet consequential cortical microstructural abnormalities in dementia with Lewy bodies, particularly in concert with Alzheimer’s disease-related changes. Their rigorous approach has advanced the neuroimaging field, unveiled potential biomarkers for improved clinical differentiation, and deepened understanding of neurodegenerative disease interplay. This landmark work heralds enhanced diagnostic precision and paves the way for innovative, targeted therapeutic regimens that could transform patient outcomes in overlapping dementia syndromes.
As the global population ages and the prevalence of neurodegenerative disorders escalates, studies like these emphasize the critical need for continued investment in advanced imaging research and neuropathological analysis. Collaboration across neuroscientific disciplines, coupled with emerging technologies, holds the promise to unravel the complexities of dementia pathophysiology and catalyze breakthroughs in treatment. The meticulous re-examination and refinement stand testament to the evolving nature of scientific discovery and its profound impact on human health.
Subject of Research: Cortical microstructural abnormalities in dementia with Lewy bodies and their associations with Alzheimer’s disease copathologies
Article Title: Author Correction: Cortical microstructural abnormalities in dementia with Lewy bodies and their associations with Alzheimer’s disease copathologies
Article References:
Mak, E., Reid, R.I., Przybelski, S.A. et al. Author Correction: Cortical microstructural abnormalities in dementia with Lewy bodies and their associations with Alzheimer’s disease copathologies. npj Parkinsons Dis. 11, 209 (2025). https://doi.org/10.1038/s41531-025-01068-y
Image Credits: AI Generated