In a groundbreaking advancement in Alzheimer’s disease research, scientists have uncovered a pivotal role of the complement protein C1q in modulating neuroinflammation and bridging the pathogenic connection between amyloid-β plaques and tau neurofibrillary tangles. This discovery, recently published in Translational Psychiatry, sheds new light on the molecular underpinnings of Alzheimer’s disease and challenges prevailing paradigms, opening fresh avenues for targeted therapeutic interventions.
Alzheimer’s disease, a progressive neurodegenerative condition marked by cognitive decline and memory loss, is hallmarked by the accumulation of amyloid-β peptides and tau protein aggregates in the brain. Although the pathological roles of these two proteins have been extensively studied, the mechanisms linking their interplay and the resulting neuroinflammatory responses remain enigmatic. The new findings implicate complement C1q, a classical initiator of the innate immune cascade, as a critical mediator in this pathogenic axis.
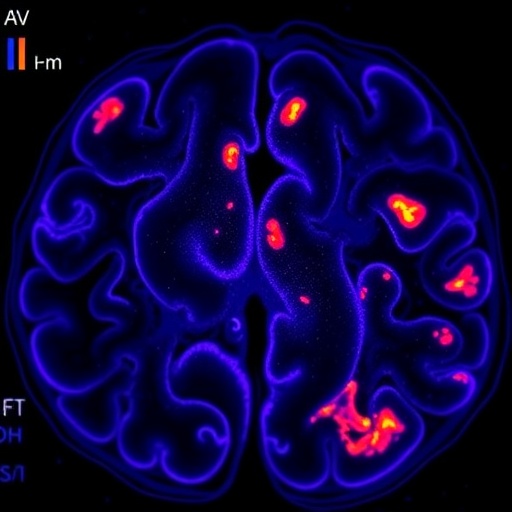
Through comprehensive molecular and histological analyses of postmortem human brain tissues and animal models of Alzheimer’s, the research team demonstrated that C1q is markedly upregulated in regions burdened with both amyloid-β deposits and tau pathology. This elevation of C1q correlates with increased microglial activation and the amplification of neuroinflammatory signaling pathways, thus suggesting a mechanistic role in exacerbating neural damage.
The complement system, traditionally recognized for its role in immune defense against pathogens, is now increasingly appreciated for its involvement in synaptic pruning and neuroimmune regulation. Within the central nervous system, C1q mediates the classical complement cascade, facilitating opsonization and clearance of cellular debris. However, aberrant activation of this pathway can foster chronic inflammation and contribute to neuronal loss. The current study compellingly positions C1q at the crossroads between protein aggregation and inflammation, potentially acting as a fulcrum driving disease progression.
Delving deeper, the investigators applied advanced imaging and biochemical techniques to unravel how C1q physically and functionally interacts with amyloid-β and tau proteins. The results suggest that C1q not only binds to amyloid-β aggregates but also enhances tau phosphorylation, a key step in tau’s pathogenic transformation. This dual engagement promotes a self-sustaining cycle where amyloid-β deposition triggers C1q-dependent inflammation, which then exacerbates tau pathology, culminating in synaptic dysfunction and neuronal demise.
Importantly, the study’s causative experiments utilizing genetic and pharmacological inhibition of C1q activity revealed a pronounced attenuation of neuroinflammation and a reduction in tau hyperphosphorylation. These interventions also improved cognitive performance in Alzheimer’s model mice, underscoring the therapeutic potential of targeting the complement cascade to disrupt the deleterious amyloid-β–tau interplay.
This comprehensive approach combining human brain analyses with mechanistic animal studies not only confirms the pathological significance of complement-mediated neuroinflammation but also positions C1q as a viable biomarker reflecting disease stage and severity. Given the heterogeneity of Alzheimer’s pathology across individuals, measuring C1q levels might guide personalized treatment strategies and monitor patient response to emerging complement-targeted therapies.
The implications of this research extend beyond a mere association between innate immunity and Alzheimer’s disease. By delineating the molecular conduit linking amyloid-β and tau via C1q, the study challenges the historically amyloid-centric model and advocates for a more integrative understanding of neurodegeneration. This paradigm shift may reshape therapeutic priorities by emphasizing immune modulation alongside amyloid and tau clearance.
Moreover, the elucidation of C1q’s role invites exploration into the temporal dynamics of complement activation across disease progression. Future longitudinal studies are needed to determine whether C1q upregulation precedes cognitive decline or serves as a downstream effector, a distinction crucial for optimal intervention timing. Additionally, dissecting how C1q’s interactions differ in early versus late stages could reveal windows of opportunity for maximal therapeutic benefit.
Scientifically, the findings call attention to the delicate balance the complement system maintains in the central nervous system, highlighting the perils of chronic complement activation amid neurodegeneration. Research into the precise signaling pathways downstream of C1q in microglia and neurons may unveil novel targets to decouple harmful inflammation from physiological immune surveillance.
Clinically, this research invigorates ongoing efforts to devise complement inhibitors with improved brain penetrance and safety profiles. Several pharmaceutical candidates targeting various complement components are in development, but fine-tuning specificity to avoid compromising host defense remains a challenge. The identification of C1q as a central player motivates renewed screening of compounds that can selectively attenuate its deleterious activity without systemic immunosuppression.
In sum, the study represents a seminal contribution to Alzheimer’s research by positioning complement C1q as a crucial nexus in the pathological dialogue between amyloid-β, tau, and neuroinflammation. This insight crystallizes an integrated model of disease pathogenesis that intertwines proteinopathy and immune dysregulation, thereby expanding the horizon of potential therapeutic strategies. As populations worldwide face the escalating burden of Alzheimer’s disease, such discoveries are invaluable in the quest for effective treatments.
The road ahead demands rigorous validation of these findings in diverse cohorts, alongside the refinement of C1q-targeted modalities. Combining complement inhibitors with existing anti-amyloid and anti-tau therapies could yield synergistic benefits, potentially halting or even reversing disease progression. Importantly, this approach advocates for personalized medicine, tailoring interventions to individuals’ immune profiles and pathological stages.
Together, these pioneering insights reverberate across neuroscience and immunology fields, emphasizing the intricate interplay between immune components and neurodegenerative processes. The study’s multidisciplinary methodology, integrating molecular biology, neuropathology, and behavioral neuroscience, exemplifies the innovative approaches needed to unravel Alzheimer’s complex etiology.
Ultimately, the revelation of complement C1q’s central role offers a hopeful prospect: by unmasking the immune mechanisms that fuel amyloid-β and tau pathology, researchers can devise smarter, more effective therapies to combat one of humanity’s most devastating diseases. As research advances, the convergence of immunology and neurodegeneration promises to revolutionize how Alzheimer’s disease is understood, diagnosed, and treated in the near future.
Subject of Research: Alzheimer’s disease pathology; neuroinflammation; complement system; amyloid-β and tau protein interaction.
Article Title: Complement C1q is associated with neuroinflammation and mediates the association between amyloid-β and tau pathology in Alzheimer’s disease.
Article References:
Guo, F., Sheng, ZH., Fu, Y. et al. Complement C1q is associated with neuroinflammation and mediates the association between amyloid-β and tau pathology in Alzheimer’s disease. Transl Psychiatry 15, 247 (2025). https://doi.org/10.1038/s41398-025-03458-5
Image Credits: AI Generated