In a groundbreaking study published in BMC Endocrine Disorders, a research team led by Shao et al. has unveiled significant findings regarding the prediction of hypoglycemia in non-intensive care unit (ICU) inpatients with diabetes. Handling the complex nature of diabetes management, which includes monitoring blood glucose levels, insulin administration, and lifestyle factors, the researchers have compared traditional logistic regression models with the increasingly popular artificial neural networks (ANNs) to determine which method best predicts hypoglycemic events. This study provides insights not merely important for healthcare professionals but offers implications for patient safety and improved diabetes management protocols that can save lives.
Hypoglycemia—a condition characterized by abnormally low blood glucose levels—can lead to serious health issues ranging from confusion to loss of consciousness and, in extreme cases, could be fatal. For inpatients with diabetes, particularly those not closely monitored in an ICU setting, the risk of hypoglycemic events is a daunting challenge. The identification of reliable predictive models is essential for clinicians. In this pursuit, logistic regression has been a long-standing statistical method employed in the medical field. However, with advancements in technology and computing, artificial neural networks have emerged as a powerful alternative.
The comparative analysis conducted by Shao and colleagues extensively documented the performance metrics of both prediction models. The researchers gathered a comprehensive dataset from a cohort of non-ICU inpatients managing diabetes. This included demographic data, clinical histories, and continuous glucose monitoring results. By structuring their analysis on this wealth of information, they aimed to reveal which model could offer a more accurate forecasting of hypoglycemic episodes. The results were nothing short of remarkable.
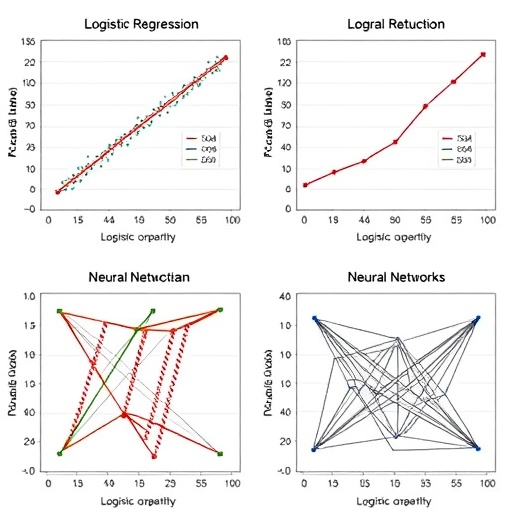
Utilizing logistic regression’s traditional statistical approach, the researchers faced challenges related to the model’s assumptions and limitations when handling complex, non-linear relationships inherent in biological data. Traditional models usually involve assumptions of linearity and independence, which in many cases do not hold true. This led to the examination of the capabilities of ANNs, which possess the ability to learn from data through layers of interconnected nodes that mimic the human brain function. Such capabilities rendered them potentially superior for detecting patterns and relationships in complex datasets.
The findings from the study highlighted that the artificial neural network model outperformed traditional logistic regression in terms of predictive accuracy and sensitivity. The researchers pointed out that ANNs were able to identify subtleties in the patterns of glucose fluctuations that logistic regression models simply missed due to their rigid structure. This aspect is crucial in clinical settings where rapid decision-making can significantly affect patient outcomes. For instance, the ability to predict a hypoglycemic event hours before it occurs could enable timely interventions, reducing the likelihood of harm to patients.
Moreover, the study incorporated a comprehensive discussion about the potential implementation of these advanced statistical methods into everyday clinical practices. The authors advocated for training healthcare professionals on the use of ANN technologies to harness their predictive strength effectively. They emphasized the importance of translating complex statistical outputs into actionable insights that clinicians can readily apply in their decision-making processes.
In addition to predictive accuracy, the researchers also explored other dimensions of model performance, including specificity and predictive values. By dissecting these components, they presented a holistic view of how both models operated under real-world conditions. This discussion provided clarity to practitioners regarding the strengths and weaknesses of each methodology. Understanding these facets is vital for integrating advanced predictive modeling into clinical pathways.
Moreover, the implications for patient safety and quality of care cannot be understated. With the right tools, healthcare professionals can anticipate hypoglycemic events and implement effective interventions, such as patient education on recognizing early warning signs, adjusting medication dosages, or tailoring dietary recommendations. This proactive approach would not only enhance patient outcomes but also contribute to a more robust healthcare system overall.
Shao et al.’s research emphasizes the need for ongoing innovation in predictive modeling within the medical field. While logistic regression will continue to have its place, especially in scenarios where data may be limited or clearly defined, the potential of artificial neural networks opens new avenues for exploration. As digital health technologies continue to evolve, the interplay between clinical practice and data science will likely deepen, highlighting the necessity for healthcare professionals to remain agile and informed.
The study concluded with a call to action for future research efforts to broaden the scope beyond hypoglycemia prediction. The authors noted that similar methodologies could be applied to other complications of diabetes and chronic diseases at large, paving the way for a new era of individualized patient care driven by advanced analytics.
In summary, this research represents a significant contribution to the ongoing battle against diabetes-related complications. By shedding light on the comparative efficacy of logistic regression and artificial neural networks, the authors have opened the door for innovative patient management strategies that could redefine how healthcare providers interact with data. As more healthcare institutions embrace technological advancements, the promise of improved patient outcomes through predictive modeling is becoming a tangible reality.
As healthcare continues to adapt to the rapid pace of technological advancements, research like that conducted by Shao et al. will remain pivotal. The continued evolution of predictive analytics could serve to empower both healthcare providers and patients, transforming the challenge of chronic disease management into an opportunity for improved outcomes. Ultimately, harnessing these sophisticated methodologies could contribute profoundly to the quality of care, ensuring that vulnerable patient populations receive the attention and intervention they need.
Subject of Research: Hypoglycemia prediction in non-ICU inpatients with diabetes
Article Title: Comparison of logistic regression and artificial neural network models for predicting hypoglycemia in non-ICU inpatients with diabetes
Article References:
Shao, F., Lin, G., Zeng, F. et al. Comparison of logistic regression and artificial neural network models for predicting hypoglycemia in non-ICU inpatients with diabetes.
BMC Endocr Disord (2025). https://doi.org/10.1186/s12902-025-02125-6
Image Credits: AI Generated
DOI: 10.1186/s12902-025-02125-6
Keywords: Hypoglycemia, diabetes, artificial neural networks, logistic regression, predictive modeling, patient safety.