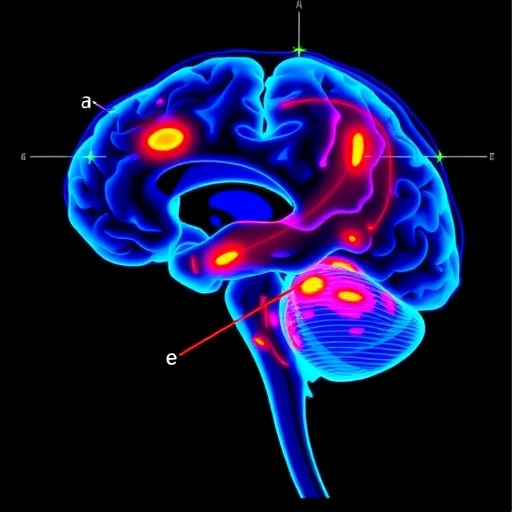
Hoboken, N.J., May 12, 2025 — Epilepsy is one of the most prevalent neurological disorders globally, impacting over 70 million individuals. In the United States alone, around 3.4 million people endure the weight of this formidable condition. While antiepileptic medications effectively control seizures for many, approximately one third of epilepsy cases remain elusive to pharmacological treatment. For those profoundly affected, surgical intervention to resect the epileptogenic zone (EZ)—the specific brain area involved in seizure generation—emerges as a promising pathway toward achieving seizure freedom, defined as a period where an individual experiences no seizures.
However, the success rates of such surgical resection hover between 50% and 60%. This shortfall can often be attributed to the challenges in precisely identifying the epileptogenic zones. To pinpoint these areas, patients typically undergo an array of diagnostic tests, including magnetic resonance imaging (MRI), electroencephalography (EEG), and intracranial EEG monitoring. Epileptologists, specialists in the management of epilepsy, leverage the data gleaned from these tests, along with descriptions of seizure semiology—symptoms and behaviors exhibited during seizures—to hypothesize the location of the EZs.
Nonetheless, a significant hurdle remains in the form of inconsistency in the language employed by different epilepsy centers. Feverish debates and variations in terminology to describe seizure semiology can convolute the communication of critical diagnosis. “Different epilepsy centers may use different terms describing the same seizure semiology,” states Feng Liu, an Assistant Professor at Stevens Institute of Technology’s Department of Systems and Enterprises. He illustrates this variability with examples such as “asymmetric posturing” versus “asymmetric tonic activity,” both referring to similar postures where one limb extends while the counterpart flexes. Such semantic discord presents considerable challenges for surgical teams, who rely on these descriptions for critical preoperative assessments.
Advancements in natural language processing have paved the way for the employment of Large Language Models (LLMs) like ChatGPT, which are trained on vast datasets comprising public medical records. These models hold the potential to bridge gaps in terminology and facilitate more accurate identification of epileptogenic zones. Liu and his team’s research investigates ChatGPT’s clinical efficacy in interpreting and analyzing seizure semiology descriptions to predict EZ locations.
In their study, the research team surveyed five board-certified epileptologists, requesting them to respond to an online questionnaire consisting of 100 questions focused on localizing the EZs based on specific semiological descriptions. Concurrently, ChatGPT was tasked with the same questions, enabling a comparative analysis of the AI’s performance against that of human experts. Findings from the study indicated that in terms of predicting the common locations of EZs, such as the frontal and temporal lobes, ChatGPT’s responses often matched or exceeded the accuracy of the epileptologists.
However, the human experts outperformed ChatGPT in predicting the locations of EZs in areas where seizures are less frequently located, such as the insula or cingulate cortex. The dualistic findings highlight the strengths and limitations of both human expertise and artificial intelligence in the domain of epilepsy surgery. These promising insights underscore the need for a multifaceted approach when utilizing AI for clinical decision-making in the context of complex medical conditions.
To augment the potential of LLMs further, Liu and his team have developed EpiSemoLLM, the first LLM fine-tuned explicitly for interpreting seizure semiology. Hosted on a specialized Stevens GPU server, this innovative platform serves as a robust decision-support tool during the pre-surgical assessment phases for neurosurgeons and epileptologists. The expectation is that the deployment of such a tailored LLM can offer an unprecedented level of precision in identifying EZs, ultimately enhancing the surgical outcomes for patients with epilepsy.
“Our findings suggest that LLMs and fine-tuned versions may act as an invaluable resource in the preoperative evaluation process for epilepsy surgery,” concludes Liu. He envisions a synergistic collaboration between skilled clinicians and artificial intelligence, positing that the intersection of human acumen and AI’s data-driven insights can yield vastly superior results in patient care. By forging this partnership, the healthcare community may unlock new frontiers in the management of epilepsy and other neurological disorders.
The ramifications of this research extend far beyond the operating table, pointing toward a future where advanced AI tools not only elevate clinical decision-making but also empower medical professionals with enhanced analytical capabilities. This convergence of technology and medicine beckons an era where the identification and treatment of challenging neurological conditions become more effective, personalized, and ultimately more humane.
Navigating the complexities of communication within epilepsy care calls for innovative solutions, and as more research elucidates the possibilities, the promise of AI-integrated medical practices seems closer than ever. For those living with epilepsy, the hope for improved treatment paradigms and increased seizure freedom may one day rest not just in the hands of specialists, but within the realm of artificial intelligence.
Subject of Research: Utilization of Large Language Models to Interpret Seizure Semiology for Epileptogenic Zone Localization
Article Title: AI-Powered Language Models Show Promise in Identifying Epileptogenic Zones in Epilepsy Patients
News Publication Date: 12-May-2025
Web References: Stevens Institute of Technology
References: Published in the Journal of Medical Internet Research
Image Credits: Not applicable
Keywords
Epileptogenesis, Epilepsy, Neurological Disorders, AI, Language Models, Seizure Semiology.