In a significant advancement in critical care medicine, a recent study has uncovered the predictive value of a novel index derived from C-reactive protein (CRP), albumin, and lymphocyte counts for assessing the risk of multiple organ failure syndrome (MOFS) in elderly patients suffering from sepsis. This condition, which poses a severe threat to physiological stability, especially in older adults, is characterized by the systemic inflammatory response that leads to organ dysfunction. The findings highlight the potential for using biochemical markers to stratify risk and tailor treatment for this vulnerable patient population effectively.
As sepsis continues to be a leading cause of morbidity and mortality in healthcare settings, understanding the pathophysiology and identifying prognostic factors is crucial. The research team led by Fan and colleagues developed the CRP-albumin-lymphocyte index, hypothesizing that these markers could serve as integrative indicators of the inflammatory state and nutritional status of patients, which are both critical in the context of sepsis. The biochemical interplay between these parameters provides insight into the underlying mechanisms of organ failure, potentially guiding clinical decision-making in real-time.
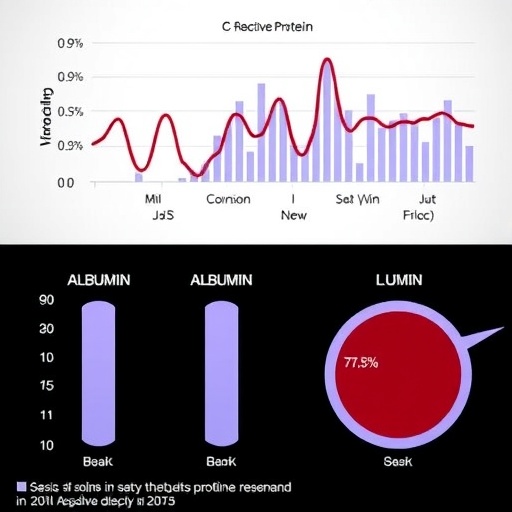
High levels of CRP are indicative of systemic inflammation, often leading clinicians to focus on managing the inflammatory response to sepsis. The role of albumin, a vital protein responsible for maintaining oncotic pressure and a marker of nutritional status, further complicates this picture—its depletion is often seen in critically ill patients. Lymphocyte counts, on the other hand, signify immune function and are frequently compromised during severe infections. By integrating these three key markers, the new index offers a multifaceted approach to assessing patient risk.
In their study, the authors meticulously analyzed data from a cohort of elderly patients diagnosed with sepsis, employing statistical models to correlate the CRP-albumin-lymphocyte index with clinical outcomes. The results indicated a strong association between elevated values of the index and adverse outcomes, including the incidence of multiple organ failure. By establishing threshold levels that define increased risk, clinicians may be positioned to intervene more proactively, possibly preventing the cascade of organ dysfunction that characterizes severe sepsis.
Moreover, the implications of this research extend beyond immediate clinical applications. By standardizing the use of the CRP-albumin-lymphocyte index in the management of sepsis, healthcare systems could enhance their protocols for monitoring patients. This approach could improve time to treatment and reduce hospital stays, ultimately impacting overall healthcare costs and patient morbidity rates. Incorporating such predictive models into existing clinical pathways would require training healthcare professionals, ensuring they understand the clinical significance and application of these biomarkers.
The research has also underscored the critical need for personalized medicine—a concept that is increasingly pertinent in the management of sepsis. As the population ages and the incidence of chronic diseases rises, understanding which biomarkers accurately predict outcomes for individual patients can optimize therapeutic strategies. The CRP-albumin-lymphocyte index is a step towards realizing such tailored approaches, blending pathophysiology with actionable clinical insights.
The methodology used in this study is noteworthy. The researchers conducted a rigorous retrospective analysis, applying stringent inclusion and exclusion criteria to enrich the study’s validity. The statistical techniques employed, including multivariable logistic regression, enabled the team to adjust for confounding factors that could skew results, providing confidence in the reliability of their findings. As a result, the work establishes a foundation upon which future prospective studies can build, potentially validating the index in diverse populations.
This study further emphasizes the significance of biomarkers in understanding the trajectory of sepsis. The triad of CRP, albumin, and lymphocyte count reflects a convergence of the inflammatory response and immune competency, highlighting the dual nature of sepsis—it is both an infectious disease and a systemic inflammatory process. By leveraging advanced analytics, researchers hope to delineate more refined approaches to patient management, thus enhancing recovery prospects.
Importantly, it is crucial to recognize the limitations inherent in any single study. The CRP-albumin-lymphocyte index, while promising, requires validation across various settings to confirm its robustness. Variability in laboratory methods, patient demographics, and the definitions of sepsis can influence outcomes, necessitating a cautious approach in the interpretation of findings. Future research should prioritize multi-center trials to strengthen the evidence base and assess the index’s performance across different clinical environments and populations.
Finally, the broader impact of these findings cannot be overstated. As the global burden of sepsis continues to escalate, driven by factors such as antibiotic resistance and the rise of comorbidities, the healthcare community must adapt. Research initiatives like this one shine a light on the potential for existing biomarkers to revolutionize patient management in critical care settings. With advancements in our understanding of sepsis pathology and the implementation of predictive models, the future holds promise for improving outcomes in some of the most critically ill patients.
In conclusion, the emergence of the CRP-albumin-lymphocyte index heralds a new era in sepsis management, especially among the elderly—a demographic significantly impacted by the condition. By marrying scientific inquiry with clinical practicality, this research underscores the imperative to refine our approaches to diagnosing and treating sepsis, thereby potentially safeguarding the lives of those most vulnerable. The implications of this study extend far beyond theoretical frameworks, promising tangible benefits to patients and healthcare providers alike.
Subject of Research: The predictive value of biochemical markers for assessing multiple organ failure syndrome in elderly patients with sepsis.
Article Title: Predictive Value of C-Reactive Protein-Albumin-Lymphocyte Index for Multiple Organ Failure Syndrome in Elderly Patients with Sepsis.
Article References:
Fan, Z., Zhang, Y., Liu, S. et al. Predictive Value of C-Reactive Protein-Albumin-Lymphocyte Index for Multiple Organ Failure Syndrome in Elderly Patients with Sepsis. Biochem Genet (2025). https://doi.org/10.1007/s10528-025-11282-1
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s10528-025-11282-1
Keywords: sepsis, C-reactive protein, albumin, lymphocyte, multiple organ failure syndrome, elderly patients, predictive model, biomarkers.