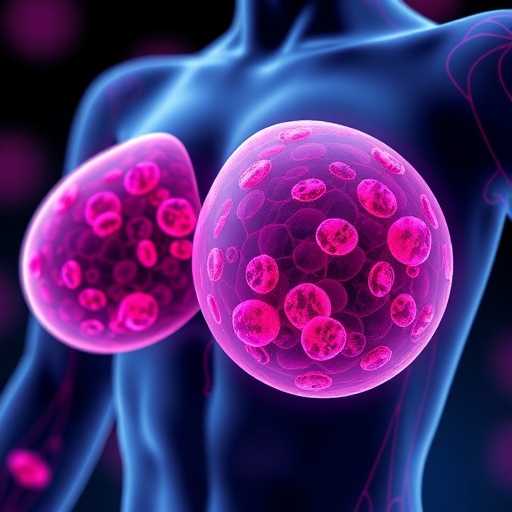
In a groundbreaking discovery that unveils the intricate metabolic interplay between cancer cells and their surrounding environment, scientists at the University of California, San Francisco have identified a novel mechanism by which triple-negative breast cancer (TNBC) cells exploit nearby fat cells to fuel their aggressive growth. This study reveals how tumor cells create direct molecular channels known as gap junctions, penetrating adipocytes to siphon vital energy in the form of lipids, essentially orchestrating an energy heist that sustains tumor proliferation.
Triple-negative breast cancer, a particularly lethal subtype characterized by the absence of estrogen, progesterone, and HER2 receptors, has long challenged oncologists due to its resistance to targeted therapies. The UCSF team observed a striking phenomenon: as the tumor expands, the surrounding fat cells visibly diminish in size, hinting at a metabolic crosstalk that enables cancer cells to tap into local energy reserves. This visual cue prompted a deeper investigation into the cellular communications facilitating this resource transfer.
The researchers discovered that TNBC cells establish gap junctions—specialized intercellular conduits that enable direct cytoplasmic exchange—into neighboring adipocytes. Through these molecular tunnels, tumor cells transmit signals that trigger the breakdown of stored fats in adipocytes, releasing free fatty acids into the tumor microenvironment. These liberated lipids are then absorbed by cancer cells, providing an abundant energy source critical for their rapid division and metastatic potential.
At the heart of this metabolic symbiosis lies the formation of gap junctions composed primarily of connexin proteins, which serve as conduits for the transfer not only of ions and small molecules but now revealed, crucial metabolic substrates. This channel formation signifies a sophisticated adaptation by malignancies to manipulate their niche, allowing them to circumvent traditional nutrient limitations and exploit neighboring tissues to their advantage.
Intriguingly, when the UCSF scientists experimented with pharmacological blockers that disrupt gap junction communication, they observed a marked inhibition of tumor growth in preclinical models. This finding positions gap junction blockade as a promising therapeutic avenue, particularly for combating the otherwise treatment-refractory TNBC. Notably, while such drugs are currently under clinical evaluation for brain cancers, their repurposing for breast cancer treatment could herald a new era of metabolic-targeted oncology.
Dr. Andrei Goga, the senior author and a professor of cell and tissue biology at UCSF, emphasized the significance of this discovery by underscoring that cancers thrive by hijacking endogenous body energy pathways, and the elucidation of this metabolic hijacking brings novel insights into TNBC biology. The study illuminates a previously underappreciated facet of tumor-host interaction and opens doors to innovative intervention strategies.
Methodologically, these breakthroughs were achieved through a combined analysis of adipose and tumor samples obtained from breast cancer patients, coupled with sophisticated in vitro and in vivo breast cancer models. These multi-level approaches allowed researchers to confirm the existence of gap junction-mediated lipid transfer and its functional implications on tumor progression, giving credence to the translational potential of their findings.
The energy harvested from adipocytes through gap junctions predominantly consists of fatty acids liberated by the enzymatic lipolysis initiated by tumor-secreted signals. This metabolic reprogramming supports critical bioenergetic and biosynthetic requirements of cancer cells, facilitating not only growth but also the invasive and metastatic behaviors that render TNBC so deadly.
Clinically, the implications of these findings are profound. Current TNBC treatment paradigms focus on chemotherapy and immunotherapy, with limited efficacy and considerable toxicity. The identification of gap junctions as metabolic conduits creates a tangible target for therapy that could disrupt tumor energetics without directly attacking cancer cells, potentially minimizing collateral damage to normal tissues.
Furthermore, the study advocates for the evaluation of gap junction inhibitors, already in trials for other malignancies, as viable candidates for breast cancer therapeutics. Given the urgency to address the aggressive nature of TNBC, integrating metabolic barrier strategies could significantly impact patient outcomes.
This research was generously supported by funding from the U.S. Department of Defense and the National Institutes of Health, among other distinguished bodies, highlighting the collaborative effort and recognition of the critical need to innovate in breast cancer research.
The unraveling of this tumor-adipocyte metabolic axis punctuates an expanding understanding of the tumor microenvironment’s role in cancer biology. It underscores the imperative to view tumors as complex ecosystems, where malignant cells co-opt normal physiological processes to ensure their survival and proliferation.
As the scientific community digests these insights, the hope is that they will galvanize further investigations into the molecular choreography of gap junction formation and function, ultimately catalyzing the development of new classes of anti-cancer drugs that specifically target these intercellular interactions.
Subject of Research: Triple-negative breast cancer metabolism and tumor microenvironment interaction
Article Title: Cancer Cells Exploit Fat Cells through Gap Junctions to Drive Aggressive Breast Tumor Growth
News Publication Date: August 20, 2024
Web References:
- UCSF Helen Diller Family Comprehensive Cancer Center
- Nature Communications Journal
Keywords: Breast cancer, Triple-negative breast cancer, Adipocytes, Gap junctions, Tumor metabolism, Tumor microenvironment, Lipid transfer, Cancer energetics, Drug therapy, Clinical trials