In a groundbreaking advancement for psychiatric neuroscience, researchers have unveiled new insights into the neuroimaging markers that define aberrant brain activity in schizophrenia. This pivotal study focuses on the complex brain dynamics underlying treatment response, a domain that has long posed challenges for clinicians and neuroscientists alike. By harnessing state-of-the-art neuroimaging techniques combined with sophisticated computational analysis of brain complexity, the authors have illuminated patterns previously obscured in the enigmatic landscape of schizophrenia.
Schizophrenia is a profoundly debilitating mental disorder characterized by disruptions in thought processes, perceptions, and emotional responsiveness. Despite decades of research, its neurobiological substrates remain only partially understood. Importantly, responses to antipsychotic treatments vary widely among patients, complicating prognosis and personalized care. In this context, the current research steps beyond conventional neuroimaging paradigms, exploiting measures of brain complexity such as entropy and fractal dimensions to quantify the disorder’s neural signatures more accurately.
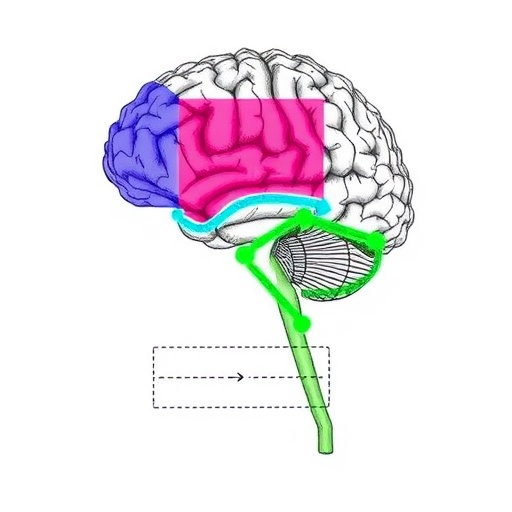
The study employed an integrative multimodal neuroimaging framework, incorporating functional MRI (fMRI) and electroencephalography (EEG) data to capture brain activity across spatial and temporal scales. By analyzing these rich data sets through advanced complexity metrics, the researchers delineated distinctive patterns of dysregulation in cortical and subcortical circuits known to govern cognitive and emotional processing. These aberrations were correlated with varying degrees of symptom severity and, crucially, differential treatment responsiveness.
One of the most striking findings emerged from the analysis of the brain’s intrinsic activity networks. Contrary to traditional models that view dysfunction as localized, the study highlighted abnormalities in the brain’s global dynamic repertoire. This entailed reduced neural complexity and diminished flexibility in network configurations, which are believed to underpin hallmark cognitive impairments in schizophrenia. The research thereby reinforces the notion that schizophrenia is a disorder of disrupted neural complexity rather than isolated neuronal anomalies.
Beyond diagnostic implications, the exploration of brain complexity yielded predictive biomarkers for therapeutic outcomes. Patients exhibiting higher baseline complexity metrics responded more favorably to antipsychotic medication, suggesting that complexity might serve as a surrogate measure of neural adaptability. This opens a promising avenue towards precision psychiatry, where individualized neuroimaging profiles could guide treatment selection and optimize clinical trajectories.
Central to the study’s innovation was the application of nonlinear dynamics and information theory principles to brain data. Traditional linear models often fail to capture the intricate and chaotic nature of brain activity. By applying entropy analysis, fractal dimension assessments, and multifractal spectrum evaluations, the researchers transformed raw neuroimaging signals into quantifiable indices of complexity. These indices proved highly sensitive to subtle pathophysiological variations across patient populations, thus enhancing the granularity of neuropsychiatric investigations.
Moreover, the correction published in Translational Psychiatry underscores the meticulous rigor with which the authors approached data integrity and interpretability. This commitment to scientific precision reinforces the reliability of the reported neuroimaging markers and supports their translational potential in clinical practice. Future iterations of this work may incorporate longitudinal designs and larger cohorts to validate and refine these markers further.
The implications of this research extend well beyond schizophrenia. By establishing robust links between brain complexity and psychiatric symptomatology, this approach may catalyze breakthroughs in understanding other neuropsychiatric disorders characterized by dysregulated neural dynamics, such as bipolar disorder, major depressive disorder, and autism spectrum disorder. This paradigm shift signals a transformative era in psychiatric diagnosis and therapy, grounded in computational neuroscience and precision medicine.
Technological advancements in both imaging hardware and computational methods have been instrumental to this research. High-resolution fMRI scanners, optimized EEG acquisition systems, and powerful algorithms for data preprocessing and analysis have allowed researchers to extract meaningful signals from complex neural datasets. The interdisciplinary collaboration among neuroscientists, clinicians, and computational experts epitomizes the integrative approach needed to tackle the complexities of brain disorders.
Importantly, this work highlights the need for a paradigm shift in psychiatric research methodologies. Traditionally, the focus has been on symptom-based categorical diagnoses rather than objective neurobiological markers. By prioritizing neuroimaging markers derived from brain complexity analyses, this study advocates for a biomarker-driven framework. Such a framework promises enhanced early detection, improved monitoring of disease progression, and tailored therapeutic interventions.
Clinically, the incorporation of neuroimaging complexity markers could revolutionize patient management workflows in psychiatry. For instance, clinicians might employ these markers to stratify patients, predict longitudinal outcomes, or customize medication regimens. This would represent a significant advance over current empirical treatment strategies, which often rely heavily on trial and error.
Further research directions involve integrating these neuroimaging findings with genetic, epigenetic, and environmental data to achieve a comprehensive understanding of schizophrenia pathogenesis. Multimodal data fusion approaches could unravel the intricate gene-brain-behavior relationships driving illness trajectories, ultimately informing more effective preventive and intervention strategies.
In summary, the study presented by Liu, Li, Kong, and colleagues offers a seminal contribution to the field by bridging the gap between neuroimaging-derived brain complexity metrics and clinical outcomes in schizophrenia. Its methodological sophistication and translational ambitions provide a blueprint for future interdisciplinary endeavors aiming to decode the complexity of the human brain in health and disease.
As psychiatric research embraces the opportunities afforded by big data, machine learning, and advanced neuroimaging, the elucidation of neural complexity markers stands out as a compelling frontier for therapeutic innovation and precision medicine. This study has not only deepened our mechanistic understanding of schizophrenia but also set the stage for next-generation diagnostics and personalized treatment paradigms that could dramatically improve patient lives.
The scientific community eagerly anticipates further validation and expansion of these findings, as such advances hold profound promise for mitigating the burden of schizophrenia globally. By redefining the neurobiological substrates of mental illness, this pioneering research paves the way towards an era where psychiatric disorders are understood with unprecedented clarity and addressed with unparalleled efficacy.
Subject of Research: Neuroimaging markers of aberrant brain activity and treatment response in schizophrenia patients based on brain complexity.
Article Title: Correction: Neuroimaging markers of aberrant brain activity and treatment response in schizophrenia patients based on brain complexity.
Article References: Liu, L., Li, Z., Kong, D. et al. Correction: Neuroimaging markers of aberrant brain activity and treatment response in schizophrenia patients based on brain complexity. Transl Psychiatry 16, 37 (2026). https://doi.org/10.1038/s41398-026-03805-0
Image Credits: AI Generated