In the relentless pursuit of groundbreaking cancer therapies, a novel twist in the complex battle against tumor immune evasion has emerged from the laboratories of Sarkar, Jiang, and Kalluri. Their recent study, published in Cell Research (2025), unveils a remarkable strategy targeting nicotinamide N-methyltransferase (NNMT) within tumor-associated fibroblasts—a discovery that reawakens lethargic T cells and revitalizes the body’s intrinsic antitumor immunity. This revelation not only deepens our understanding of the tumor microenvironment but also opens an innovative therapeutic avenue that could revolutionize current immunotherapy paradigms.
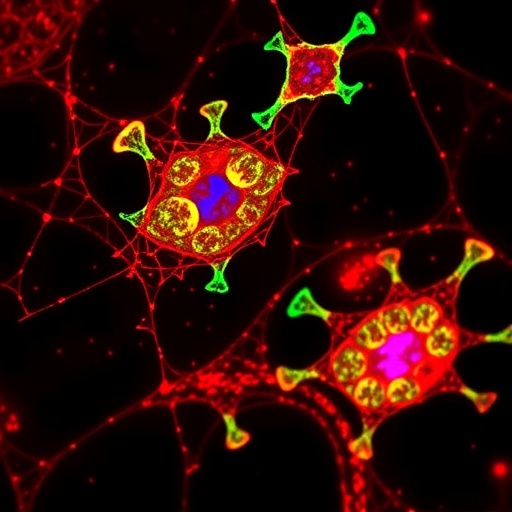
The tumor microenvironment (TME) has long been recognized as a principal barrier undermining the efficacy of immune responses against cancer. It is a dense and intricate ecosystem composed of cancer cells alongside a diverse repertoire of stromal cells, immune subsets, and molecular signals—a milieu that collectively orchestrates immune suppression and tumor progression. Among these constituents, fibroblasts—stromal cells that give structural and biochemical support—have recently surfaced as pivotal modulators capable of dictating the pace and success of immune engagement against tumors.
Sarkar and colleagues directed their investigative lens on NNMT, an enzyme notoriously overexpressed in cancer-associated fibroblasts (CAFs). NNMT catalyzes the methylation of nicotinamide, a key player in cellular metabolism and epigenetic regulation within the TME. The upregulation of NNMT in fibroblasts has been previously linked to the promotion of a pro-tumoral phenotype, yet its direct role in immune modulation remained ambiguous until now. The authors meticulously delineated how NNMT acts as a molecular gatekeeper suppressing cytotoxic T cell function, effectively placing a brake on the immune system’s natural tumor-fighting machinery.
Experimentally, the team harnessed sophisticated genetic ablation and pharmacological inhibition techniques to selectively silence NNMT in fibroblasts within tumor-bearing mouse models. This targeted approach yielded profound immunological shifts: the previously exhausted CD8+ T cells regained their proliferative and cytotoxic capacities, culminating in robust antitumor responses. The once “cold” tumors devoid of significant immune infiltration rapidly transformed into inflamed “hot” tumors teeming with activated T cells capable of mounting effective eradication of cancerous cells.
Delving deeper into the mechanistic underpinnings, the researchers uncovered that NNMT activity reprograms fibroblast metabolism in a way that fosters an immunosuppressive microenvironment. This metabolic rewiring involves alterations in key metabolites that influence the epigenetic landscape, modulating gene expression patterns that promote fibroblast-mediated T cell suppression. By interrupting this cascade, NNMT inhibition alleviates metabolic constraints, thereby restoring a milieu conducive to T cell activation and infiltration.
Importantly, this metabolic-epigenetic axis appears to intersect with immune checkpoint pathways, rendering the tumor microenvironment more responsive to existing immunotherapies such as PD-1/PD-L1 blockade. The combinatorial potential of NNMT targeting alongside checkpoint inhibitors synergistically amplified antitumor immunity, suggesting a promising therapeutic synergy. This insight is particularly critical given the limited success of checkpoint blockade in tumors characterized by dense fibroblast networks and immune exclusion.
The translational implications of these findings extend beyond murine models, as comprehensive analyses of human tumor specimens revealed elevated NNMT expression within fibroblasts across diverse cancer types, correlating with poor patient prognosis and diminished T cell infiltration. This reinforces the clinical relevance of NNMT as a biomarker of immune suppression and a viable target for therapeutic intervention. Current or future NNMT inhibitors, some already under preclinical development, could therefore serve as adjunct therapies to reinvigorate antitumor immunity in patients refractory to conventional treatments.
Moreover, the revelation that tumor stroma—the traditionally overlooked “scaffold” of cancer—actively manipulates immune responses through metabolic enzymes underscores a paradigm shift in oncology research. The findings entrench fibroblasts at the center of immunomodulatory dynamics and build a compelling case for the integrated targeting of stromal metabolism to complement immunotherapy. Recognizing and dismantling the metabolic defenses erected by CAFs may be the key to unlocking durable cancer regression.
This study also sheds light on the broader field of cancer immunometabolism, a domain exploring how metabolic pathways within both tumor and immune cells influence disease progression and therapy outcomes. NNMT emerges as a central node linking metabolism and epigenetics within the stromal compartment, presenting untapped opportunities to reshape the TME and sensitize tumors to immune assault through metabolic recalibration.
Considering the structurally and functionally diverse fibroblast populations within tumors, future research is warranted to delineate the specific CAF subsets expressing NNMT and their distinct roles in immune suppression. Such heterogeneity could dictate differential responses to NNMT-targeted therapies and require precision medicine approaches to identify patients most likely to benefit from this intervention.
Beyond oncology, the role of NNMT in fibroblast biology may have implications for fibrotic diseases, where aberrant fibroblast activation contributes to pathological tissue remodeling. Thus, the mechanistic insights from this study might transcend cancer immunology, offering new angles for therapeutic innovations in inflammatory and fibrotic disorders.
Furthermore, challenges remain in the efficient delivery and specificity of NNMT inhibitors to the fibroblast compartment within the TME. Nanoparticle-based drug delivery systems or antibody-drug conjugates targeting fibroblast-specific markers could be explored to enhance targeting precision and minimize off-target effects, thereby maximizing therapeutic benefit.
In conclusion, the pioneering work of Sarkar, Jiang, and Kalluri spotlights NNMT in fibroblasts as a linchpin of tumor immune evasion and a compelling candidate for therapeutic targeting. By reawakening dormant T cells and dismantling stromal-imposed immunosuppression, NNMT inhibition heralds a new frontier in immuno-oncology where metabolic and stromal components are harnessed to reinvigorate antitumor immunity. This integrated approach could reshape clinical strategies and ultimately improve survival outcomes for patients battling resistant and immunologically “cold” cancers.
As the oncology community grapples with the complexities of immune evasion, the convergence of metabolism, epigenetics, and stromal biology embodied in NNMT research promises to unlock latent immune potentials within the tumor microenvironment. Continued exploration and clinical translation of these insights stand to transform cancer treatment and offer fresh hope for millions worldwide confronting this formidable disease.
Subject of Research:
Molecular mechanisms by which nicotinamide N-methyltransferase (NNMT) expression in tumor-associated fibroblasts modulates T cell activity and tumor immunity, focusing on metabolic and epigenetic reprogramming within the tumor microenvironment and implications for cancer immunotherapy.
Article Title:
Targeting NNMT in fibroblasts reawakens T cells and restores antitumor immunity
Article References:
Sarkar, M., Jiang, Y. & Kalluri, R. Targeting NNMT in fibroblasts reawakens T cells and restores antitumor immunity. Cell Res (2025). https://doi.org/10.1038/s41422-025-01181-w
Image Credits: AI Generated