In a groundbreaking study published in Cell Death Discovery, researchers have unveiled a novel therapeutic avenue that could reshape the approach to Parkinson’s disease (PD), one of the most debilitating neurodegenerative disorders worldwide. The investigation centers on the inhibition of bone morphogenetic protein (BMP) signaling within astrocytes, revealing a potent mechanism to mitigate neuroinflammation, a critical factor exacerbating PD pathology. This revelation could herald a paradigm shift by targeting glial cells, rather than neurons alone, opening new frontiers for PD management.
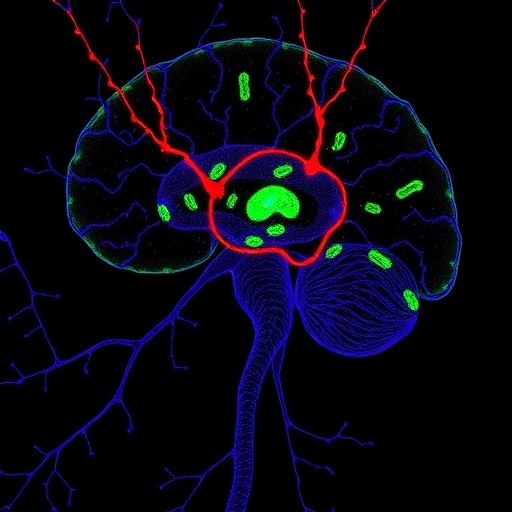
Parkinson’s disease is characterized by the progressive loss of dopaminergic neurons in the substantia nigra, which leads to classic motor symptoms such as tremors, rigidity, and bradykinesia. However, an increasing body of evidence highlights the substantial role of neuroinflammation in the progression of PD. Astrocytes, the star-shaped glial cells in the brain, have been traditionally seen as supportive players in maintaining neuronal homeostasis. Yet, their contribution to the neuroinflammatory response and subsequent neuronal damage in PD is now drawing significant attention.
The study led by Li et al. delves deeply into how astrocyte BMP signaling exacerbates neuroinflammation in experimental Parkinson’s models. BMPs, part of the transforming growth factor-beta (TGF-β) superfamily, regulate numerous cellular processes ranging from development and differentiation to immune responses. Within the brain’s cellular milieu, aberrant BMP signaling in astrocytes appears to amplify inflammatory cascades that accelerate neuronal injury, thus worsening PD pathology.
Using genetically engineered mouse models and in vitro cellular systems, the researchers demonstrated that suppressing BMP signaling specifically in astrocytes effectively dampened the neuroinflammatory response. This attenuation correlated with reduced microglial activation, decreased release of inflammatory cytokines, and importantly, preservation of dopaminergic neurons within the substantia nigra. The specificity of targeting astrocytes avoids potentially disruptive interference with BMP pathways in other critical cell types.
Mechanistically, the inhibition of astrocytic BMP signaling downregulated the expression of pro-inflammatory markers such as interleukin-1β (IL-1β), tumor necrosis factor-alpha (TNF-α), and inducible nitric oxide synthase (iNOS). This reduction in inflammatory mediators curtailed the vicious cycle of neuroinflammation that propagates neuronal damage. Additionally, amelioration of astrocyte reactivity brought about favorable changes in neuronal microenvironment, promoting neuroprotection and potentially facilitating endogenous repair mechanisms.
This research further elucidated the downstream molecular cascades associated with BMP signaling in astrocytes, highlighting the critical roles of SMAD proteins—key intracellular effectors of BMP receptors. The study’s data suggest that suppressing SMAD phosphorylation disrupts the transcriptional programs responsible for promoting a pro-inflammatory astrocyte phenotype. These insights add precision to how BMP pathway inhibitors might be fine-tuned to achieve optimal therapeutic benefits without compromising essential physiological functions.
Translationally, the authors tested pharmacological inhibitors of BMP signaling and observed parallel neuroprotective effects, strengthening the case for clinical exploration. Given the multiplicity of pathogenic pathways in PD, this novel strategy targeting astrocyte-mediated neuroinflammation presents a complementary approach alongside existing dopamine replacement therapies and emerging disease-modifying agents.
Moreover, this study emphasizes the evolving understanding of glia-neuron interactions in neurodegenerative disorders. Astrocytes are no longer passive bystanders but active modulators of neuroinflammation and neuronal survival. Targeting astrocyte signaling networks could unlock new dimensions in therapeutic development not only for PD but potentially for other neurodegenerative diseases where inflammation plays a pivotal role, such as Alzheimer’s disease and multiple sclerosis.
The research also probes the timing and progression of astrocyte BMP signaling involvement in PD. The findings imply that early intervention to suppress astrocytic BMP activity may forestall or slow the neurodegenerative cascade. This temporal aspect is critical for the design of clinical trials aiming to deploy BMP pathway modulators effectively in patients at early or prodromal PD stages.
Critically, the study raises important questions about the safety profile and long-term impacts of inhibiting BMP signaling in the central nervous system. BMPs contribute to vital processes like neurogenesis and synaptic plasticity, warranting cautious dissecting of therapeutic windows to mitigate potential off-target effects. Future research will need to address how to balance suppressing harmful inflammation while preserving essential physiological functions within the brain.
The work by Li et al. also offers a powerful paradigm for leveraging advanced genetic tools and molecular profiling to tease apart intricate signaling networks in specific brain cell populations. Their approach demonstrates how cell-type specific interventions can achieve targeted modulation of pathogenic pathways, a principle that could revolutionize therapeutic strategies across neurological disorders.
In sum, the discovery that astrocyte BMP signaling inhibition significantly alleviates neuroinflammation provides a compelling new dimension to combat Parkinson’s disease. By shifting focus to glial biology and steering away from neuron-centric paradigms, this study illuminates fresh therapeutic perspectives that could ultimately enhance quality of life and outcomes for millions affected by PD globally.
As the field moves forward, combination strategies integrating BMP pathway modulators with neuroprotective and symptomatic treatments might emerge as robust approaches to slow disease progression and improve motor and non-motor symptoms, addressing the multifaceted nature of Parkinson’s. The research invites a reimagining of glial cells from mere support units to dynamic players whose modulation holds the key to impactful neurodegenerative disease therapy.
Continued exploration into BMP signaling nuances, the interplay with other inflammatory mediators, and clinical trial design will be essential to translate these foundational findings into effective, safe treatments. This landmark study is not only a beacon for Parkinson’s research but a call to broaden our understanding of brain cell communication networks in health and disease, unlocking the potential of next-generation neurotherapeutics.
Subject of Research: Parkinson’s disease and neuroinflammation, focusing on astrocyte BMP signaling
Article Title: Inhibition of astrocyte BMP signaling alleviates neuroinflammation in experimental models of Parkinson’s disease
Article References:
Li, Y., Hao, J., Wang, W. et al. Inhibition of astrocyte BMP signaling alleviates neuroinflammation in experimental models of Parkinson’s disease. Cell Death Discov. 11, 528 (2025). https://doi.org/10.1038/s41420-025-02812-2
Image Credits: AI Generated
DOI: 10 November 2025