In a groundbreaking study published on November 3, 2025, scientists have unveiled the therapeutic potential of antler stem cell-derived exosomes in combating the destructive effects of diabetic periodontitis. This research opens a new frontier in periodontal treatment by harnessing the regenerative capabilities of a naturally occurring biological agent. The investigation, conducted on a rat model, showcases how these exosomes can restore periodontal homeostasis by enhancing reactive oxygen species (ROS) scavenging and promoting osteogenesis, which are critical processes for maintaining healthy gum tissue and bone structure.
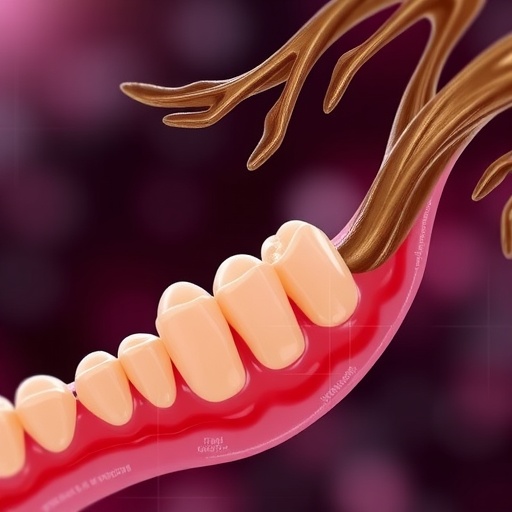
Diabetic periodontitis, a severe complication in patients with uncontrolled diabetes, is characterized by chronic inflammation, oxidative stress, and irreversible bone loss around teeth. Traditional treatments have often fallen short in reversing these pathological changes, largely due to the intricate interplay between oxidative stress and impaired bone regeneration. The novel approach utilizing antler stem cell-derived exosomes offers a dual mechanism of action, precisely targeting these pathological hallmarks.
At the cellular level, exosomes are extracellular vesicles secreted by many cell types that facilitate intercellular communication by transferring proteins, lipids, and nucleic acids. The researchers isolated these vesicles specifically from antler stem cells, which are known for their remarkable regenerative capacity due to the aggressive and rapid growth of deer antlers. By leveraging the inherent biological potency of these exosomes, the study aimed to test their efficacy in neutralizing ROS and fostering new bone formation.
The research team used a rat model with experimentally induced diabetic periodontitis to closely mimic the human disease condition. The rats demonstrated characteristic signs of increased oxidative stress and alveolar bone loss, making them ideal candidates to evaluate the efficacy of the exosomal therapy. Upon administration, the exosomes facilitated a significant reduction in ROS levels, which ordinarily exacerbate tissue damage and inflammatory responses. This antioxidant role is pivotal because oxidative stress is a major driver of periodontal degradation in diabetic patients.
Additionally, the study demonstrated that the antler stem cell-derived exosomes enhanced osteogenesis—the process by which new bone is formed. Bone regeneration in periodontitis is notoriously difficult due to the chronic inflammatory microenvironment that impairs the differentiation and function of osteoblasts. The vesicles appear to stimulate osteoprogenitor cells and modulate inflammatory mediators, thereby creating a conducive environment for bone repair. This finding underscores the therapeutic promise of exosome-based interventions for reversing bone loss associated with chronic periodontal disease.
One of the remarkable aspects of this research lies in its ability to integrate anti-inflammatory and antioxidant effects with regenerative processes. The exosomes not only suppress detrimental free radicals but also activate signaling pathways that promote tissue regeneration. This dual-action approach could potentially lead to more effective clinical outcomes compared to therapies that only focus on controlling infection or inflammation.
Mechanistically, the study revealed that the exosomes carried a cargo of microRNAs and proteins critical to cellular antioxidant responses and bone metabolism. These bioactive molecules influenced key signaling networks such as the nuclear factor erythroid 2-related factor 2 (Nrf2) pathway, which regulates cellular defense against oxidative damage. Activation of Nrf2 resulted in the upregulation of antioxidant enzymes, tipping the balance away from oxidative stress toward tissue preservation and regeneration.
From a translational perspective, the use of antler stem cell-derived exosomes presents a novel and potentially safer therapeutic avenue as opposed to cell transplantation. Exosome therapy circumvents many of the risks associated with stem cell therapies, including immune rejection and tumorigenicity, while maintaining the ability to modulate the cellular environment favorably. This approach reflects an emerging paradigm in regenerative medicine focused on cell-free strategies.
Moreover, the study’s findings could impact not only diabetic periodontitis but also other diseases characterized by oxidative stress and bone loss, such as osteoporosis and rheumatoid arthritis. The inherent antioxidative and osteogenic properties of these exosomes provide a versatile platform for future therapeutic development in musculoskeletal medicine.
The researchers noted the importance of further investigations to optimize exosome dosage, delivery methods, and long-term safety profiles before clinical trials in humans can be initiated. Nonetheless, the current findings represent a significant milestone in periodontal and regenerative medicine, offering hope for millions suffering from diabetes-related oral complications.
The implications of this research extend beyond therapy to diagnostic applications. Exosomes can serve as biomarkers for disease progression and treatment response, given their reflective molecular cargo of parental cells. Understanding these exosomal signatures could pave the way for personalized medicine approaches in managing diabetic periodontitis and similar inflammatory bone diseases.
In conclusion, the study by Guo, Ren, Libonati, and colleagues is a seminal contribution that demonstrates the restorative potential of antler stem cell-derived exosomes in diabetic periodontitis. By effectively scavenging ROS and promoting osteogenesis, these exosomes restore periodontal homeostasis, presenting a novel therapeutic strategy that merges the advantages of natural regenerative cues with modern biomedical technology. This approach holds promise not only for dental medicine but also for broader applications in tissue engineering and regenerative therapies.
As the scientific community continues to explore the multifaceted roles of exosomes, their utility in addressing complex systemic and localized pathologies will undoubtedly expand. This pioneering work stands as a testament to the power of nature-inspired solutions in advancing human health and combating chronic debilitating diseases.
Future research directions outlined by the authors include exploring the molecular mechanisms underlying exosome-mediated immunomodulation and bone repair in diabetic environments, as well as integrating exosome therapy with current periodontal treatment modalities to enhance efficacy and clinical outcomes. Such multidisciplinary efforts will accelerate the transition from bench to bedside, revolutionizing the management of diabetes-related periodontal destruction.
This discovery also invites a reevaluation of stem cell-derived exosome sources, highlighting antler stem cells as a uniquely potent reservoir for regenerative factors. Considering the regenerative ability of antlers, exosomes from this source might harbor novel biomolecules absent in other cell types, offering unexpected therapeutic benefits.
Ultimately, this study reinforces the critical role of oxidative stress in diabetic complications and positions antioxidant strategies alongside regenerative medicine as a next-generation approach to treatment. The convergence of these fields, exemplified by antler stem cell-derived exosomes, marks an exciting chapter in biomedical research with profound clinical implications for millions worldwide.
Subject of Research: Therapeutic effects of antler stem cell-derived exosomes on diabetic periodontitis, focusing on ROS scavenging and osteogenesis in a rat model.
Article Title: Antler stem cell-derived exosomes restore periodontal homeostasis in a rat model with diabetic periodontitis through enhancing ROS scavenging and osteogenesis.
Article References:
Guo, Q., Ren, S., Libonati, A. et al. Antler stem cell-derived exosomes restore periodontal homeostasis in a rat model with diabetic periodontitis through enhancing ROS scavenging and osteogenesis. Cell Death Discov. 11, 500 (2025). https://doi.org/10.1038/s41420-025-02800-6
Image Credits: AI Generated
DOI: 10.1038/s41420-025-02800-6