In a revolutionary stride for neurodegenerative disease research, a team of scientists has unveiled a groundbreaking therapeutic strategy aimed at spinal muscular atrophy (SMA), a devastating genetic disorder characterized by progressive muscle wasting and weakness. Published in Nature Communications, this latest study demonstrates the transformative potential of targeted antisense oligonucleotide (ASO) treatment to rescue developmental abnormalities in spinal muscular atrophy organoids, heralding new hope for patients and families afflicted by this condition. This report delves into the technical intricacies and profound implications of this pioneering approach.
Spinal muscular atrophy is primarily caused by mutations in the survival motor neuron 1 (SMN1) gene, leading to insufficient levels of the SMN protein crucial for motor neuron survival. The deficit of this protein triggers a cascade of events culminating in motor neuron degeneration and muscle atrophy. Traditional treatments have focused on symptom management or partially compensating for the loss of SMN protein but have fallen short of fully reversing disease progression. The study at hand breaks new ground by utilizing organoids—three-dimensional, miniaturized, and simplified versions of organs grown in vitro—to model the intricacies of early neuronal development affected by SMA.
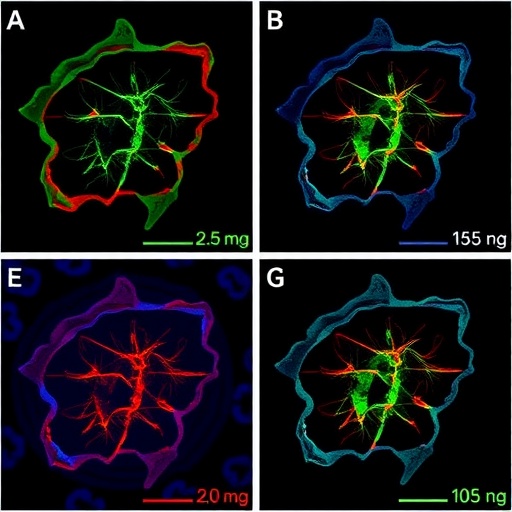
Organoids provide an unprecedented window into human neurodevelopment, bridging the gap between traditional two-dimensional cell cultures and live animal models. They recapitulate many features of the human spinal cord’s architecture and cellular diversity, allowing researchers to observe the exact developmental defects caused by SMA mutations. The research team leveraged this platform to test the efficacy of antisense oligonucleotides designed to modulate RNA splicing and upregulate functional SMN protein production in these organoids.
Antisense oligonucleotides are short strands of synthetic nucleic acids engineered to specifically bind RNA transcripts, altering their splicing or stability. In the context of SMA, ASOs can enhance the inclusion of exon 7 in the SMN2 gene transcript, a nearly identical gene to SMN1, thereby increasing the production of a functional protein variant to compensate for SMN1 loss. The team’s approach involved delivering these ASOs into spinal organoids derived from patient-specific induced pluripotent stem cells, mimicking the disease environment in a controlled laboratory setting.
At the molecular level, the study revealed that ASO treatment successfully restored the correct splicing pattern in SMN2, manifesting as elevated SMN protein levels within the organoids. This biochemical correction translated into robust phenotypic improvements: the previously observed developmental delays and morphological aberrations in motor neuron progenitors were significantly ameliorated. Detailed imaging and electrophysiological analyses underscored enhanced neuronal maturation and synaptic functionality, marking a pivotal reversal of the cellular hallmarks of SMA.
Furthermore, transcriptomic profiling provided deep insights into the gene expression landscape altered by SMA and its subsequent rescue. Prior to treatment, the organoids exhibited widespread dysregulation of genes implicated in neuronal differentiation, axonal guidance, and synapse formation pathways. Remarkably, ASO intervention realigned these gene expression profiles closer to those observed in healthy controls, illuminating the broad-reaching impact of SMN protein restoration beyond motor neurons alone.
One of the most striking outcomes of this research is the demonstration that targeted ASO therapy can correct developmental defects during the critical phases of neurogenesis. This finding challenges previous assumptions that SMA alterations are irreversible postnatally and opens new avenues for early therapeutic intervention, potentially even prenatally. By defining a developmental window amenable to correction, the study adds invaluable knowledge for clinicians and researchers strategizing treatment timelines.
From a translational perspective, the use of patient-derived organoids ensures that the therapeutic effects observed are relevant to human physiology, bolstering the likelihood of success in clinical settings. This model system also allows for the testing of personalized medicine approaches, tailoring ASO sequences to individual genetic backgrounds to maximize efficacy and minimize off-target effects. The research team emphasizes that while the road to clinical application will require extensive validation and safety assessments, their findings establish a robust framework for future SMA therapies.
This study also underscores the technological advancements enabling precise delivery and cellular uptake of antisense oligonucleotides within complex tissue systems. The successful penetration of ASOs into densely packed organoid structures without inducing cytotoxicity is a testament to improved chemical modifications and delivery vectors, which will be crucial in scaling these treatments to human patients. Such innovations are at the forefront of modern molecular medicine, transforming once theoretical concepts into tangible therapeutics.
Moreover, the implications extend beyond SMA, as the methodological framework combining organoid technology with ASO modulation can be potentially adapted to other neurodevelopmental and neurodegenerative disorders caused by splicing defects or gene dysregulation. Diseases such as amyotrophic lateral sclerosis, certain forms of epilepsy, and even Alzheimer’s disease might benefit from similar RNA-targeted correction strategies, accelerating the burgeoning field of RNA therapeutics.
Ethical considerations accompany these exciting advancements, especially with the use of stem cell-derived human tissue models. The ability to simulate human neurological development in vitro provides a powerful tool, yet it also demands a thoughtful discourse on the boundaries of organoid use, including questions about complexity, sentience, and long-term culturing. The research team acknowledged these concerns, emphasizing transparency and adherence to evolving guidelines governing stem cell research.
From a broader scientific communication perspective, the integration of cutting-edge genomic editing technologies like CRISPR/Cas9 with organoid and ASO therapies represents a synergy poised to revolutionize personalized medicine. While this study focused on antisense oligonucleotides, future research may combine multiple modalities to enhance therapeutic outcomes, creating bespoke treatments for a spectrum of genetic diseases with precision and minimal invasiveness.
In essence, this breakthrough marks a paradigm shift in our understanding and treatment of spinal muscular atrophy—moving from symptom palliation to molecular correction within a physiological context that mimics human development. The ability to rescue motor neuron development in a dish not only accelerates drug discovery pipelines but also inspires hope that similar approaches can transform the prognosis of countless individuals worldwide burdened by SMA.
As research continues to unravel the intricate layers of SMA pathophysiology, this study stands out as a beacon demonstrating that the union of molecular genetics, bioengineering, and regenerative medicine is no longer an abstract ideal but a practical reality. The extraordinary collaboration among molecular biologists, neurologists, bioengineers, and data scientists has catalyzed an innovative solution with profound implications for the future of neuromuscular therapy.
Finally, it is worth noting that the study’s publication in a prestigious, peer-reviewed journal lends credence to its rigor and scientific merit, ensuring that the findings undergo meticulous scrutiny by the global community. The promise shown by targeted ASO treatment in patient-derived organoids may soon translate into clinical trials, bringing the field one step closer to changing lives beyond the laboratory confines.
This mesmerizing advancement not only illustrates the power of precision medicine but also exemplifies the relentless human quest to conquer neurological diseases at their genetic roots. As we stand on the cusp of a new era in SMA treatment, the world watches with anticipation as science converts hope into healing.
Subject of Research: Spinal Muscular Atrophy developmental alterations and targeted antisense oligonucleotide treatment.
Article Title: Targeted antisense oligonucleotide treatment rescues developmental alterations in spinal muscular atrophy organoids.
Article References:
Faravelli, I., Rinchetti, P., Tambalo, M. et al. Targeted antisense oligonucleotide treatment rescues developmental alterations in spinal muscular atrophy organoids. Nat Commun (2025). https://doi.org/10.1038/s41467-025-67725-1
Image Credits: AI Generated