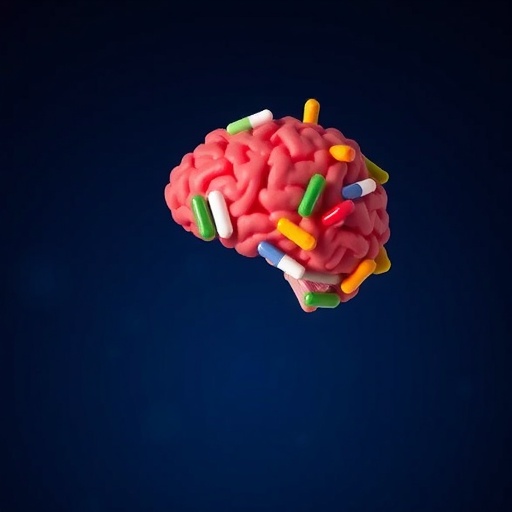
In a groundbreaking scoping review published in Translational Psychiatry this November, researchers have embarked on a novel exploration of the neurocognitive effects of Alzheimer’s disease (AD) medications on children and adolescents diagnosed with autism spectrum disorder (ASD) who also exhibit low intelligence quotient (IQ). This pioneering inquiry bridges two seemingly disparate domains of neuropharmacology, opening new avenues for therapeutic strategies targeting cognitive impairments within the ASD population, a subgroup long underserved by conventional treatment models.
The rationale behind this study stems from the underlying neuropathological and neurochemical commonalities observed between Alzheimer’s disease and certain neurodevelopmental disorders. While Alzheimer’s primarily affects aging populations with hallmark features of memory decline and executive dysfunction, autism spectrum disorder is characterized by pervasive developmental challenges in social interaction, communication, and repetitive behaviors, often coupled with cognitive deficits. Notably, shared aspects such as synaptic dysfunction, neuroinflammation, and neurotransmitter imbalances suggest potential overlapping mechanisms that could be modulated by similar pharmacological agents.
Employing a comprehensive scoping review framework, the research team systematically assessed existing literature for evidence of AD medications’ impacts on neurocognitive outcomes in ASD youth with low IQ. Alzheimer’s treatments, particularly cholinesterase inhibitors and glutamate receptor modulators, have well-documented efficacy in enhancing synaptic plasticity and cognitive function in adults, but their utility in pediatric populations with distinct neurodevelopmental profiles remains largely unexplored. By navigating through the intricacies of diverse clinical trials, observational studies, and case reports, the researchers sought to map the current knowledge landscape and identify promising directions for future clinical research.
At the core of the review lies a critical examination of cholinesterase inhibitors—drugs that increase levels of acetylcholine, a neurotransmitter pivotal for learning and memory. These agents, such as donepezil and rivastigmine, have revolutionized Alzheimer’s care by partially restoring cholinergic signaling pathways impaired in dementia. Intriguingly, cholinergic dysfunction has also been implicated in ASD, suggesting potential neurochemical targets that could yield cognitive benefits. Preliminary clinical data suggest heterogenous responses, ranging from subtle improvements in attention and executive function to minimal adverse events, thereby warranting cautious optimism.
Glutamatergic neurotransmission, another focal pathway in AD pharmacotherapy, has drawn attention for its dual role in synaptic plasticity and excitotoxicity. Memantine, an NMDA receptor antagonist, acts by modulating aberrant glutamate activity to protect neurons from damage while preserving cognitive function. Its off-label application in ASD has sporadically demonstrated enhancements in behavioral symptoms and adaptive functioning, though results remain inconsistent across studies. The review highlights the mechanistic underpinnings of memantine and analogous compounds that could recalibrate excitatory-inhibitory balance—often disrupted in autism—with potential downstream effects on cognition.
In addition to monotherapies, the interplay of combined pharmacological strategies is considered critical for optimizing neurocognitive outcomes. The multifaceted nature of ASD, compounded by low IQ, necessitates a nuanced approach that addresses diverse neural circuits and compensatory mechanisms. The review underscores the imperative for rigorous clinical trial designs incorporating robust cognitive assessments, biomarker analyses, and longitudinal follow-up to disentangle the precise contributions of AD medications in this context.
Importantly, the researchers emphasize the considerable ethical and developmental considerations intrinsic to pharmacological interventions in pediatric neurodevelopmental disorders. The potential for adverse effects on the developing brain, alongside the variability in individual neurobiology, mandates a judicious evaluation of risk-benefit ratios. The review advocates for stratified medicine approaches, leveraging genetic, neuroimaging, and neurophysiological data to tailor treatments and monitor efficacy and safety meticulously.
Highlighting gaps in the literature, the scoping review identifies a paucity of large-scale, randomized controlled trials explicitly targeting the ASD-low IQ cohort with AD medications. Most existing studies are limited by small sample sizes, heterogeneous methodologies, and primarily focus on behavioral outcomes rather than direct neurocognitive measures. This underscores an urgent need for high-powered, mechanistically informed clinical investigations to validate preliminary findings and elucidate treatment mechanisms.
Beyond pharmacology, the review contextualizes these findings within broader therapeutic landscapes, including behavioral interventions and supportive educational strategies. The integration of AD medications as adjunctive treatments could potentiate neuroplasticity and learning capacities, potentially enhancing the efficacy of comprehensive ASD programs. This aligns with emerging paradigms advocating for multimodal, interdisciplinary approaches to optimize functional outcomes in neurodevelopmental disorders.
Technological advances in biomarker discovery and neuroimaging are poised to accelerate progress in this domain. Functional MRI, PET scans targeting cholinergic and glutamatergic systems, and electrophysiological studies could provide unprecedented insights into drug action and neural circuitry alterations in response to therapy. The review calls for leveraging these tools to inform patient selection, dosing regimens, and treatment monitoring, ultimately prefacing precision medicine frameworks for ASD management.
In sum, this scoping review illuminates an innovative frontier at the intersection of neurodegeneration and neurodevelopment. It proposes that repositioning AD medications might open untapped therapeutic potentials for children and adolescents grappling with ASD and low IQ, a population confronting significant cognitive and adaptive challenges. While the evidence remains nascent and calls for robust future inquiry, this work forms a foundational reference point for clinicians, researchers, and stakeholders invested in advancing neurocognitive health across the lifespan.
This collaborative endeavor, integrating expertise from neuropharmacology, psychiatry, and developmental neuroscience, exemplifies the translational spirit essential for tackling complex brain disorders. It underscores the imperative to transcend traditional diagnostic silos and embrace cross-disciplinary explorations that may yield transformative benefits for vulnerable populations historically marginalized in clinical research.
As the neuroscience community grapples with the complexities of autism and cognitive impairment, this review catalyzes important conversations around innovative therapeutic repurposing. It invites bold hypotheses and methodologically rigorous investigations that could redefine standards of care and improve quality of life for children and adolescents navigating the intersecting challenges of ASD and intellectual disability.
Continued investment in this nascent field promises to uncover molecular and cellular insights with far-reaching implications, potentially shedding light on convergent neuropathological pathways across diverse neuropsychiatric and neurodegenerative disorders. By harnessing the lessons learned from Alzheimer’s pharmacotherapy, the search for effective interventions in autism may gain valuable momentum, ultimately enriching our understanding and treatment of complex brain dysfunction.
The implications of such research extend beyond immediate clinical outcomes, shaping policy decisions, educational frameworks, and societal perceptions around neurodiversity and cognitive health. This paradigm shift invites a more inclusive and mechanistically grounded approach to neurodevelopmental disabilities, fostering hope and tangible progress in an area long characterized by unmet needs and therapeutic challenges.
In conclusion, this scoping review stands as a testament to innovative scientific inquiry and the promise of interdisciplinary collaboration. By rigorously evaluating the potential of Alzheimer’s disease medications to enhance neurocognitive outcomes in children and adolescents with autism spectrum disorder and low IQ, it lays critical groundwork for future breakthroughs poised to transform clinical practice and quality of life for this underserved population.
Subject of Research: Neurocognitive effects of Alzheimer’s disease medications on children and adolescents with autism spectrum disorder and low IQ.
Article Title: Effect of Alzheimer’s disease medications on neurocognitive outcomes in children and adolescents with autism spectrum disorder and low IQ: a scoping review.
Article References:
Diamandis, N., van den Anker, J.N. & Denisova, K. Effect of Alzheimer’s disease medications on neurocognitive outcomes in children and adolescents with autism spectrum disorder and low IQ: a scoping review. Transl Psychiatry 15, 475 (2025). https://doi.org/10.1038/s41398-025-03655-2
Image Credits: AI Generated
DOI: 17 November 2025