In a groundbreaking study published in Nature Communications, researchers have unveiled a novel cellular mechanism that could revolutionize our understanding of lung fibrosis, a debilitating and often fatal disease affecting millions worldwide. This intricate investigation, led by Hoffman, Shah, Barboza, and colleagues, delves into the enigmatic role of a previously uncharacterized population of intermediate alveolar epithelial cells in driving pathogenic fibroblast activation. This discovery heralds a paradigm shift in comprehending the cellular crosstalk underlying the progression of pulmonary fibrosis and offers new therapeutic targets for interventions that might halt or even reverse disease progression.
Pulmonary fibrosis is a chronic scarring disorder of the lung parenchyma that results in a progressive decline in respiratory function. Its pathogenesis is complex, involving aberrant tissue repair and fibroblast proliferation that disrupts normal alveolar architecture. Central to this pathological remodeling is the interplay between the alveolar epithelium— the thin cellular layer facilitating gas exchange— and the mesenchymal compartment, especially fibroblasts responsible for extracellular matrix deposition. While prior research has elucidated elements of this process, the precise cellular intermediates and molecular triggers initiating fibrotic cascades remained elusive.
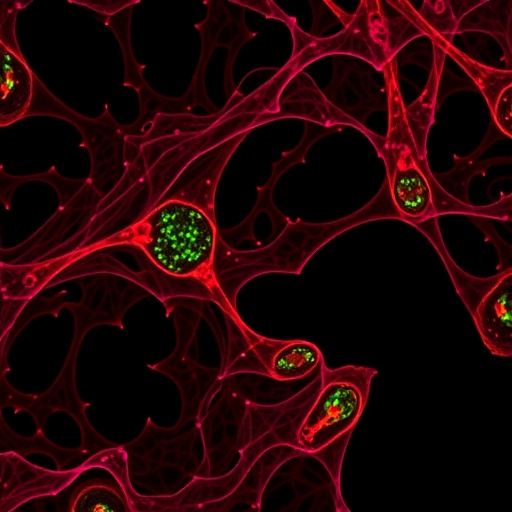
The research team employed advanced preclinical models to simulate lung fibrosis and conducted meticulous single-cell transcriptomic analyses. Their results revealed that beyond the well-known alveolar type 1 (AT1) and type 2 (AT2) epithelial cells lies a heterogenous spectrum of intermediate alveolar epithelial cells. These intermediates exhibit distinct gene expression profiles indicative of aberrant cellular states, marked by enhanced pro-fibrotic signaling signatures and secretion of factors that directly stimulate fibroblast pathogenic activation.
One of the most compelling findings is that these aberrant intermediate cells do not merely represent transitional phenotypes in normal epithelial regeneration; rather, they embody dysfunctional states that actively exacerbate fibrosis. The study delineates how these cells upregulate a cadre of cytokines, growth factors, and extracellular matrix components, effectively reprogramming fibroblasts into pathological myofibroblasts. Such myofibroblasts are the primary effector cells orchestrating fibrotic matrix deposition, tissue stiffness, and lung function impairment.
Delving deeper, the researchers identified key signaling pathways and molecular mediators exploited by aberrant intermediates to co-opt fibroblast behavior. This includes dysregulated TGF-β signaling, a cornerstone profibrotic pathway long implicated in fibrosis, but now linked explicitly to intermediate epithelial cellular states. Moreover, the cross-talk involves novel paracrine factors and extracellular vesicle-mediated communication, underscoring the complexity of epithelial-mesenchymal dialogue in fibrotic pathobiology.
Technological advances such as high-throughput single-cell RNA sequencing and spatial transcriptomics were instrumental in unraveling these intricate cellular interactions. These approaches provided unprecedented resolution, enabling the team to map the spatial distribution, temporal dynamics, and molecular characteristics of intermediate alveolar epithelial cells within fibrotic lung tissue. Their data suggest that the expansion and persistence of these intermediates in fibrotic niches are critical determinants of disease severity and chronicity.
Beyond molecular and cellular insights, the study evaluated potential therapeutic implications by targeting these aberrant intermediates. Genetic and pharmacologic interventions aimed at modulating intermediate cell emergence or function resulted in a significant attenuation of fibroblast activation and extracellular matrix deposition in preclinical fibrosis models. These promising results pave the way for novel treatment strategies that disrupt the earliest pathological events in fibrosis, ideally preventing irreversible lung damage.
Importantly, the findings raise thought-provoking questions about epithelial plasticity and its dual-edged role in tissue repair and pathology. The emergence of aberrant intermediate states implies that regenerative programs can become maladaptive under chronic injurious stimuli, leading to persistent cellular dysfunction and disease progression. Understanding the triggers and checkpoints governing this maladaptive transition is now a priority for the field.
The implications of this work extend beyond lung fibrosis. Fibrotic diseases afflict numerous organs, including the liver, kidney, and heart, where epithelial-mesenchymal interactions similarly drive pathological remodeling. The concept of aberrant intermediate epithelial cells may represent a ubiquitous fibrogenic mechanism, offering a unifying framework to tackle fibrotic disorders systemically.
As with any pioneering research, several open questions remain. The ontogeny and fate of these intermediate cells during fibrosis resolution versus progression warrant further longitudinal studies. Additionally, it will be crucial to validate these cellular phenotypes and mechanisms in human patient samples across diverse etiologies and disease stages. Such validation is essential to translate these insights into clinically actionable paradigms.
This landmark study exemplifies how integrative experimental modeling and cutting-edge molecular techniques can transform our understanding of chronic lung diseases. By illuminating the pathological role of aberrant intermediate alveolar epithelial cells, Hoffman and colleagues have opened new avenues for research and therapeutic innovation. Their contributions underscore the urgent need to move beyond symptomatic treatments toward mechanistically targeted therapies that address the cellular roots of fibrosis.
As the global burden of fibrotic lung diseases continues to rise, partly due to aging populations and environmental factors, this research offers a beacon of hope. It establishes a foundation for future efforts aiming to intercept fibrotic processes early, preserving lung function and improving patient outcomes. The scientific community will keenly follow further developments stemming from these insights.
In conclusion, the discovery of pathogenic intermediate alveolar epithelial cells marks a transformative advance in pulmonary fibrosis research. It challenges conventional paradigms of epithelial repair and fibrosis, emphasizing the nuanced and dynamic cellular ecosystems within diseased lungs. Through multidisciplinary investigation, this work heralds a new era in fibrosis biology—one that promises to unlock effective therapies for patients desperately in need.
Subject of Research: Aberrant intermediate alveolar epithelial cells and their role in lung fibrosis pathogenesis
Article Title: Aberrant intermediate alveolar epithelial cells promote pathogenic activation of lung fibroblasts in preclinical fibrosis models
Article References:
Hoffman, E.T., Shah, A., Barboza, W.R. et al. Aberrant intermediate alveolar epithelial cells promote pathogenic activation of lung fibroblasts in preclinical fibrosis models. Nat Commun 16, 8710 (2025). https://doi.org/10.1038/s41467-025-63735-1