In a significant advancement for pancreatic cancer diagnostics, researchers have unveiled a sophisticated deep learning-based model that automatically segments pancreatic solid neoplasms on MRI scans while simultaneously deploying a radiomics approach to enhance diagnostic accuracy. This cutting-edge integration promises to refine how pancreatic tumors are detected and classified, potentially transforming clinical workflows and patient outcomes in oncology.
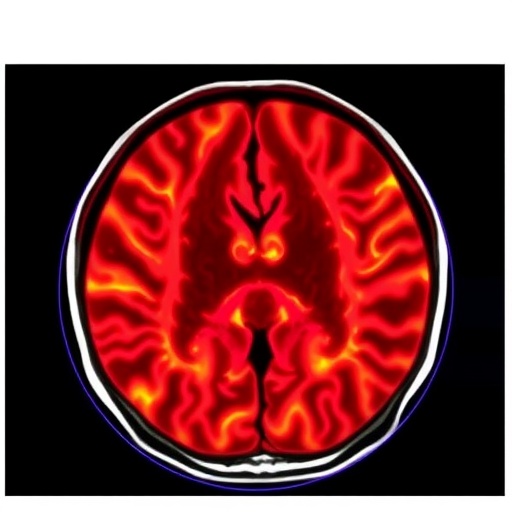
The pancreas, a vital yet elusive organ, has long posed diagnostic challenges due to the subtle nature and varied morphology of its solid neoplasms. Conventional imaging interpretation often requires expert radiologists and can involve subjective variability. The novel approach developed leverages a three-dimensional neural network architecture known as nnU-Net, which excels in medical image segmentation by learning from volumetric MRI data, allowing for precise delineation of tumor boundaries with minimal human intervention.
The study retrospectively analyzed MRI scans from patients who had undergone surgical resection for pancreatic tumors. The training dataset included 165 patients, while 89 were reserved for testing the generalizability of the model. The MRI sequences principally consisted of T2-weighted imaging (T2WI) and diffusion-weighted imaging (DWI), modalities that provide complementary tissue contrast necessary for differentiating neoplastic tissue from normal pancreatic parenchyma.
Performance evaluation of the deep learning segmentation model revealed impressive quantitative metrics, with a mean Dice Similarity Coefficient (DSC) reaching 0.82 on T2WI and an astonishing 0.91 on DWI within the training cohort. These high DSC values indicate a near-expert level of overlap between the algorithm’s predicted segmentations and manually annotated ground truths. Despite a natural performance dip in the independent testing cohort, DSCs of 0.64 on T2WI and 0.70 on DWI still underscored significant segmentation reliability.
Critically, the model’s efficacy extended to challenging sub-centimeter lesions smaller than 2 cm—a notorious blind spot in pancreatic imaging. For this subset, the algorithm maintained respectable DSC scores, achieving 0.74 on T2WI and 0.92 on DWI during training, although these metrics understandably decreased to 0.51 and 0.62 respectively when validated externally. This indicates a remarkable sensitivity to detect and outline even diminutive and subtle pancreatic tumors that might otherwise be overlooked.
Beyond mere segmentation, the researchers harnessed the segmented regions of interest (ROIs) to extract high-dimensional radiomic features, quantifiable markers of tumor heterogeneity, texture, and shape invisible to the naked eye. From these features, nine radiomics signatures were meticulously selected to construct a diagnostic classification model aiming to distinguish pancreatic ductal adenocarcinomas (PDACs) from other solid tumor types like neuroendocrine neoplasms and solid pseudopapillary neoplasms, which require different therapeutic strategies.
The radiomics model demonstrated exceptional discriminatory power, registering area under the curve (AUC) values of 0.968 during training and a robust 0.790 on the independent test set. These figures reflect outstanding diagnostic accuracy, reinforcing the model’s clinical potential to aid oncologists and radiologists in making more informed decisions, minimizing invasive biopsies, and tailoring personalized treatment paths based on a non-invasive imaging modality.
This research heralds a pivotal step forward in the integration of artificial intelligence into oncologic radiology, marking the first time a combined approach of deep learning segmentation and radiomics diagnostics has been applied specifically to pancreatic solid tumors in MRI studies. The synergy of segmentation precision and radiomic insight encapsulates the promise of AI to augment human expertise, reduce diagnostic uncertainty, and enhance reproducibility.
As pancreatic cancer is often diagnosed late due to vague symptoms and anatomical challenges, early and reliable detection is crucial to improving prognosis. Tools like this deep learning model bring hope by potentially enabling routine screening programs to automatically flag suspicious lesions and guide subsequent clinical actions promptly.
Moreover, the methodological framework established can be adapted and extended to other abdominal tumors and imaging modalities, creating a blueprint for comprehensive AI-powered diagnostic solutions in oncology. Researchers emphasize that while the current study’s performance is compelling, ongoing prospective validation, integration with clinical datasets, and refinement for small lesion detection will be essential next steps.
The fusion of deep learning-based segmentation with radiomics analysis beautifully illustrates precision medicine’s trajectory, where machine intelligence deciphers complex imaging phenotypes and translates them into actionable medical knowledge. It empowers clinicians with detailed tumor characterization beyond visual assessment, unraveling microstructural tumor properties through computational algorithms.
The study’s reliance on retrospective data and the complexity of MRI acquisition protocols do highlight limitations that encourage future multicenter collaborations to enhance standardization and robustness. Nevertheless, the demonstrated efficacy in automated tumor detection and histological differentiation with non-invasive MRI positions this technology as a transformative adjunct to current diagnostic standards.
In conclusion, this innovative deep learning and radiomics model represents a leap forward in the diagnostic landscape of pancreatic solid neoplasms. By accurately segmenting tumors and deciphering their radiomic signatures, it lays the foundation for more precise, timely, and personalized management of pancreatic cancer—a notoriously challenging disease that urgently demands improvements in early detection and diagnostic accuracy.
The promising results underscore the growing role of artificial intelligence not merely as a supplementary tool but as a fundamental component capable of reshaping oncologic imaging paradigms. As this technology matures, it may well contribute significantly to improving patient survival and quality of life by enabling clinicians to better understand tumor biology through the lens of advanced computational imaging.
The integration of such AI-driven diagnostic models into clinical practice will require collaboration between radiologists, oncologists, machine learning experts, and regulatory bodies to ensure safety, effectiveness, and ethical implementation. The future of pancreatic oncology could soon witness a revolutionary shift driven by these intelligent imaging approaches.
With pancreatic cancer remaining one of the deadliest cancers globally, innovations such as this represent beacons of hope. The capacity to detect tumors earlier, stratify their types non-invasively, and guide personalized treatment regimens has the potential to alter the typically grim prognosis associated with this malignancy.
Continued research and investment into AI-powered imaging, supported by expanding datasets and evolving algorithms, are critical to unlock the full potential of this technology. The exciting developments presented in this study demonstrate a promising horizon where machine intelligence and human expertise converge to combat pancreatic cancer and save lives.
Subject of Research: Pancreatic solid neoplasms diagnosis using deep learning segmentation and radiomics on MRI.
Article Title: Deep learning automatic segmentation and radiomics model for diagnosing pancreatic solid neoplasms in MRI.
Article References:
Shi, YJ., Zhang, H., Wang, LL. et al. Deep learning automatic segmentation and radiomics model for diagnosing pancreatic solid neoplasms in MRI. BMC Cancer 25, 1563 (2025). https://doi.org/10.1186/s12885-025-15021-y
Image Credits: Scienmag.com