In the relentless battle against ovarian cancer—the deadliest among gynecological malignancies—a novel avenue of research is providing renewed hope and a significant stride towards personalized therapy. A recent study published in BMC Cancer introduces groundbreaking insights into the use of organoid models derived from both primary tumors and patient-derived xenograft (PDX) tumors, revealing their promising capacity to accurately mirror the platinum-based chemotherapy responsiveness seen in patients. This advancement could revolutionize the therapeutic landscape, particularly for patients grappling with chemotherapy-resistant forms of ovarian cancer.
Ovarian cancer presents a daunting clinical challenge due to its typically late-stage diagnosis and the formidable obstacle of chemotherapy resistance, which significantly contributes to disease recurrence and mortality. Traditional preclinical models, while informative, have fallen short in reliably predicting patient-specific drug responses, especially concerning platinum-based agents that remain the frontline treatment. The development of patient-derived xenograft models represented a leap forward by preserving tumor genetics in vivo, yet their costly and labor-intensive nature restricts their widespread application in high-throughput drug screening.
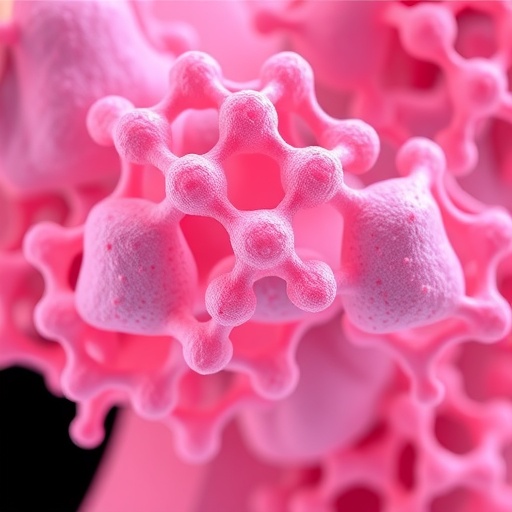
Enter the realm of organoids—three-dimensional cellular cultures recapitulating the complexity and heterogeneity of the original tumor microenvironment. These miniaturized tumor models, grown directly from patient tumor samples, preserve cellular diversity and architecture, offering an exquisite platform for investigating individualized drug responses. However, a persistent limitation has been the scarcity of primary tumor tissues available for generating these models, hindering their extensive utilization.
In a strategic approach to overcome this bottleneck, the study investigated whether organoids derived from PDX tumors (PDX-derived organoids, or PDXOs) could serve as reliable surrogates paralleling the drug sensitivity profiles of primary patient-derived organoids (PDOs). The researchers established 3D organoid cultures from malignant ascites samples obtained from five ovarian cancer patients characterized by diverse platinum sensitivity statuses—platinum-sensitive, platinum-resistant, and platinum-refractory. Matched PDX samples from both ascites and solid tumors were utilized to generate corresponding organoids, enabling a direct comparative analysis.
The organoids’ viability was assessed following treatment with paclitaxel (PTX), carboplatin (CBDCA), and their combination over a 72-hour period, reflecting standard clinical chemotherapy regimens. This allowed a rigorous evaluation of whether PDXOs can authentically replicate the drug response patterns observed in PDOs, and ultimately in the clinical scenarios of the originating patients. This methodological design ensured a robust, translationally relevant framework to validate the models’ predictive power.
Remarkably, the results demonstrated that organoids derived from primary tumors and those from PDX implanted tumors exhibited remarkably parallel drug sensitivities. Both organoid types faithfully mirrored patients’ clinical responses to platinum-based chemotherapy. For instance, organoids from platinum-sensitive patients displayed significant declines—around fifty percent—in viability following treatment with carboplatin, paclitaxel, or their combination. In clear contrast, organoids from platinum-resistant and platinum-refractory cases maintained high viability, reflecting their insensitivity to standard chemotherapy modalities.
Beyond substantiating the fidelity of PDXOs in replicating platinum sensitivity, the study also uncovered nuanced insights into organoid morphology and its relevance to drug response. Organoids derived from ascites formed smaller, denser cellular clusters compared to solid tumor-derived organoids; yet, both preserved equivalent drug response profiles. This finding emphasizes the robustness of organoid models regardless of the tumor source, expanding potential accessibility to varied clinical specimens for personalized drug testing.
An intriguing facet emerged when organoids from one platinum-resistant case responded modestly yet significantly to paclitaxel monotherapy. This observation offers a glimpse into the models’ capacity to predict differential sensitivity to second-line chemotherapeutics, a critical advancement given the limited options currently available for platinum-resistant ovarian cancer patients. Such predictive versatility could guide more precise therapeutic decisions, potentially improving outcomes for a cohort with historically poor prognosis.
The implications of this study are profound. It validates the use of PDXOs as renewable, scalable platforms for high-throughput drug screening, overcoming the scarcity of primary tissues. This is particularly pertinent for discovering novel agents targeting platinum-resistant ovarian cancers, which remain an unmet clinical challenge. By leveraging PDXOs, research can accelerate the identification and optimization of effective therapeutics tailored to individualized tumor biology.
Moreover, the study’s findings reinforce the significance of organoids as a bridge between preclinical research and clinical outcomes, underscoring their utility in personalized medicine paradigms. These models provide a dynamic, patient-specific testing ground where multiple therapeutic scenarios can be evaluated before clinical application, reducing the guesswork inherent in current treatment algorithms.
From a technical standpoint, the organoid cultures were maintained under conditions promoting three-dimensional architecture and preserving intratumoral heterogeneity. The treatment assays quantitatively assessed live-cell viability post-exposure, employing standardized metrics to ensure reproducibility and clinical relevance. Such meticulous methodology reinforces the robustness and translational potential of the findings.
This research also hints at a future where personalized ovarian cancer management may routinely incorporate organoid-based drug sensitivity testing. Integrating organoid platforms into clinical workflows could facilitate rapid identification of effective chemotherapeutic combinations, minimizing exposure to ineffective treatments and associated toxicities. The eventual goal is treatments tailored not just to tumor histology but to the functional characteristics of each patient’s unique cancer.
Additionally, the study champions the practical synergy between PDX models and organoid technology. While PDX models provide a living tumor environment that conserves genetic fidelity, organoids derived from these models combine accessibility with the capacity for high-throughput analysis. This dual approach harnesses the strengths of both systems, positioning PDXOs as invaluable tools in oncology research.
The broader implications extend beyond ovarian cancer. The successful demonstration that PDXO models reflect patient drug responses could inspire similar strategies across diverse cancer types, particularly those with limited primary tissue availability. This paradigm shift has the potential to transform preclinical drug development and accelerate personalized therapy frameworks.
Importantly, the study elucidates the biological underpinnings of chemotherapy response and resistance in ovarian cancer, offering avenues to probe mechanisms at a level previously unattainable. Understanding how tumor heterogeneity and microenvironmental factors influence drug efficacy via organoid models fosters the rational design of next-generation therapeutics.
In essence, this study represents a compelling leap forward in ovarian cancer research, aligning cutting-edge organoid technology with clinical realities. As precision medicine continues its ascent, these findings underscore the critical role of sophisticated in vitro models that reflect the complex biology of human tumors and their response to treatment.
With promising data supporting the equivalence of PDXO and PDO models in reflecting patient chemotherapy response, researchers and clinicians alike are poised to harness these platforms to improve therapeutic outcomes. The integration of such innovative models into drug development pipelines heralds a new era for ovarian cancer patient care—a future where treatment is as unique as the tumor itself.
Subject of Research: Ovarian cancer chemotherapy response; patient-derived organoid and patient-derived xenograft tumor models.
Article Title: Organoid models established from primary tumors and patient-derived xenograft tumors reflect platinum sensitivity of ovarian cancer patients.
Article References: Nikeghbal, P., Zamanian, D., Burke, D. et al. Organoid models established from primary tumors and patient-derived xenograft tumors reflect platinum sensitivity of ovarian cancer patients. BMC Cancer 25, 1459 (2025). https://doi.org/10.1186/s12885-025-14811-8
Image Credits: Scienmag.com