New York, NY [May 20, 2024]—Researchers at the Icahn School of Medicine at Mount Sinai have designed a regenerative medicine therapy to speed up diabetic wound repair. Using tiny fat particles loaded with genetic instructions to calm down inflammation, the treatment was shown to target problem-causing cells and reduce swelling and harmful molecules in mouse models of damaged skin.

Credit: Lab of Yizhou Dong, PhD, at Icahn Mount Sinai.
New York, NY [May 20, 2024]—Researchers at the Icahn School of Medicine at Mount Sinai have designed a regenerative medicine therapy to speed up diabetic wound repair. Using tiny fat particles loaded with genetic instructions to calm down inflammation, the treatment was shown to target problem-causing cells and reduce swelling and harmful molecules in mouse models of damaged skin.
Details on their findings were published in the May 20 online issue of the Proceedings of the National Academy of Sciences (PNAS).
Diabetic wounds, often resistant to conventional treatments, pose serious health risks to millions of people worldwide. Immune cells known as macrophages, which are supposed to help, end up causing inflammation instead. This inflammation harms other cells and makes it harder for the wound to heal properly and quickly.
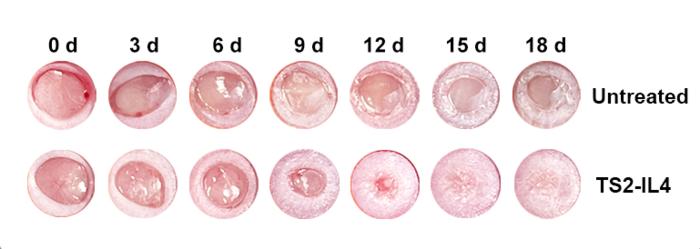
Using lipid nanoparticles (LNPs) loaded with RNA encoding IL-4, a cell-to-cell signaling protein known as a cytokine, the therapy targeted dysfunctional macrophages while simultaneously reducing inflammation and “reactive oxygen species” (ROS) in diabetic wounds.
ROS molecules are produced naturally in the body during various metabolic processes and play roles in cell signaling and immune responses. However, excessive ROS production can lead to oxidative stress, causing damage to cells, proteins, and DNA. This stress is associated with various diseases and conditions, including inflammation and aging.
“In preclinical models, we basically showed the therapy’s ability to reprogram pro-inflammatory macrophages into reparative ones, leading to improved wound healing outcomes,” says Yizhou Dong, PhD, corresponding author of the study, Professor of Immunology and Immunotherapy, and a member of the Icahn Genomics Institute and the Marc and Jennifer Lipschultz Precision Immunology Institute at Icahn Mount Sinai. ”Dysfunctional macrophages drive diabetic non-healing wounds, but we can reprogram them to stop the damage and instead help the healing process. We aim to promote faster and more effective wound closure by reprogramming these cells and modulating the inflammatory environment.”
Earlier this year, in a related study, Dr. Dong and colleagues reported on lipid nanoparticles that enhanced the tissue engineering and regeneration activity of adipose stem cells for treating diabetic wounds (Nature Communications).
While the results of the current study are encouraging, the researchers emphasize the need for a rigorous randomized controlled clinical trial to confirm safety and efficacy in humans.
“Our ultimate goal is to translate these findings into tangible benefits for diabetic patients. With further research and validation, this RNA-LNP therapy could potentially revolutionize diabetic wound management with one easily scalable application of a comparatively inexpensive therapeutic agent,” says Dr. Dong. “The study also suggests the potential for RNA-LNP therapeutics to be more generally designed to reprogram disease-causing macrophages in an organism, as pro-inflammatory macrophages are implicated in a wide range of diseases.”
The paper is titled “Accelerating diabetic wound healing by ROS-scavenging lipid nanoparticle-mRNA formulation.”
The remaining authors are Siyu Wang, PhD (Icahn Mount Sinai); Yuebao Zhang, PhD (Ohio State University); Yichen Zhong, BS (Icahn Mount Sinai); Yonger Xue, PhD (Ohio State University, Icahn Mount Sinai); Zhengwei Liu, PhD (Icahn Mount Sinai); Chang Wang, PhD (Icahn Mount Sinai); Diana D. Kang, PhD (Ohio State University, Icahn Mount Sinai); Haoyuan Li, MD (Icahn Mount Sinai); Xucheng Hou, PhD (Icahn Mount Sinai); Meng Tian, PhD (Icahn Mount Sinai); Dinglingge Cao, PhD (Icahn Mount Sinai); Leiming Wang, PhD (Icahn Mount Sinai); Kaiyuan Guo, BS (Icahn Mount Sinai); Binbin Deng, PhD (Ohio State University); David W. McComb, PhD (Ohio State University); Miriam Merad, MD, PhD (Icahn Mount Sinai); and Brian D. Brown, PhD (Icahn Mount Sinai).
The study was funded in part by the National Institute of General Medical Sciences grant R35GM144117.
To view competing interests, see the PNAS paper.
-####-
About the Icahn School of Medicine at Mount Sinai
The Icahn School of Medicine at Mount Sinai is internationally renowned for its outstanding research, educational, and clinical care programs. It is the sole academic partner for the eight- member hospitals* of the Mount Sinai Health System, one of the largest academic health systems in the United States, providing care to a large and diverse patient population.
Ranked 13th nationwide in National Institutes of Health (NIH) funding and among the 99th percentile in research dollars per investigator according to the Association of American Medical Colleges, Icahn Mount Sinai has a talented, productive, and successful faculty. More than 3,000 full-time scientists, educators, and clinicians work within and across 44 academic departments and 36 multidisciplinary institutes, a structure that facilitates tremendous collaboration and synergy. Our emphasis on translational research and therapeutics is evident in such diverse areas as genomics/big data, virology, neuroscience, cardiology, geriatrics, as well as gastrointestinal and liver diseases.
Icahn Mount Sinai offers highly competitive MD, PhD, and Master’s degree programs, with current enrollment of approximately 1,300 students. It has the largest graduate medical education program in the country, with more than 2,000 clinical residents and fellows training throughout the Health System. In addition, more than 550 postdoctoral research fellows are in training within the Health System.
A culture of innovation and discovery permeates every Icahn Mount Sinai program. Mount Sinai’s technology transfer office, one of the largest in the country, partners with faculty and trainees to pursue optimal commercialization of intellectual property to ensure that Mount Sinai discoveries and innovations translate into healthcare products and services that benefit the public.
Icahn Mount Sinai’s commitment to breakthrough science and clinical care is enhanced by academic affiliations that supplement and complement the School’s programs.
Through the Mount Sinai Innovation Partners (MSIP), the Health System facilitates the real-world application and commercialization of medical breakthroughs made at Mount Sinai. Additionally, MSIP develops research partnerships with industry leaders such as Merck & Co., AstraZeneca, Novo Nordisk, and others.
The Icahn School of Medicine at Mount Sinai is located in New York City on the border between the Upper East Side and East Harlem, and classroom teaching takes place on a campus facing Central Park. Icahn Mount Sinai’s location offers many opportunities to interact with and care for diverse communities. Learning extends well beyond the borders of our physical campus, to the eight hospitals of the Mount Sinai Health System, our academic affiliates, and globally.
——————————————————-
* Mount Sinai Health System member hospitals: The Mount Sinai Hospital; Mount Sinai Beth Israel; Mount Sinai Brooklyn; Mount Sinai Morningside; Mount Sinai Queens; Mount Sinai South Nassau; Mount Sinai West; and New York Eye and Ear Infirmary of Mount Sinai.
Journal
Proceedings of the National Academy of Sciences
Method of Research
Experimental study
Subject of Research
Animals
Article Title
Accelerating diabetic wound healing by ROS-scavenging lipid nanoparticle-mRNA formulation
Article Publication Date
20-May-2024