A groundbreaking advancement in cancer immunotherapy has emerged from researchers at the University of Basel and University Hospital Basel in Switzerland, unveiling a novel fusion protein that masterfully combines two potent therapeutic strategies into a single, sophisticated molecule. This innovative treatment simultaneously disrupts the immune evasion tactics employed by tumor cells and selectively invigorates the body’s tumor-fighting immune cells. Such dual-action design holds the promise of significantly more effective cancer therapies, potentially delivering heightened efficacy alongside a reduction in the severe side effects characteristic of many existing treatments.
The history of cancer immunotherapy is marked by remarkable milestones, none more notable than the pioneering work of Dr. Stephen Rosenberg in the early 1980s. He treated Linda Taylor, a patient diagnosed with advanced skin cancer, with an experimental interleukin-2 (IL-2)-based therapy. Taylor became the first patient to be cured using the body’s own immune system as a weapon against cancer, forever transforming the landscape of oncology. Interleukin-2, a cytokine known to promote the proliferation and activation of various immune effector cells, was later approved by the FDA as an early form of immunotherapy. Although IL-2 therapy demonstrated potent antitumor activity, it was hampered by substantial systemic toxicity and the inadvertent activation of regulatory T cells (Tregs), which paradoxically suppress immune responses.
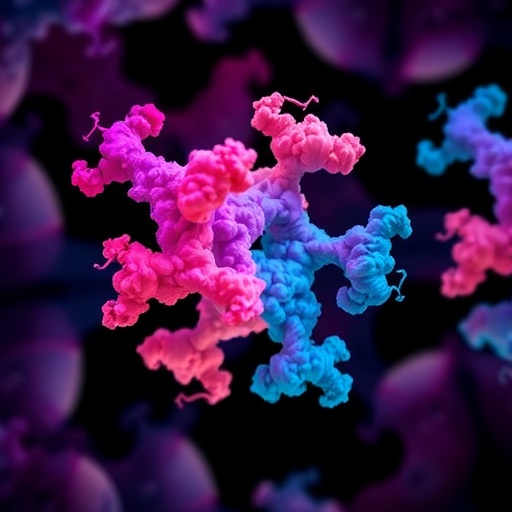
To circumvent these limitations, contemporary research has focused on engineering IL-2 variants (IL-2v) designed to preferentially activate cytotoxic immune cells, such as CD8+ T cells and natural killer (NK) cells, while sparing the immunosuppressive Tregs. The newly developed fusion protein discovered by the Basel team, and developed in collaboration with pharmaceutical giant Roche, represents a paradigm shift by coupling an IL-2v with an antibody targeting PD-1 (programmed cell death protein 1). PD-1 is a critical immune checkpoint receptor expressed on tumor-infiltrating lymphocytes, which tumors exploit to dampen immune responses and evade destruction.
The fusion protein’s architecture is ingeniously designed for cis-delivery—that is, the simultaneous localization of the IL-2 variant and the PD-1 checkpoint blockade to the exact immune cells suspended within the tumor microenvironment. This targeted approach ensures that the immune-activating cytokine reaches its intended cellular targets without inducing generalized immune stimulation, thereby lowering off-target effects and toxicity. By blocking PD-1 signaling, the antibody component lifts the inhibitory “brakes” imposed by the tumor on T cells, thus rejuvenating exhausted T cells that had become inactive through chronic antigen exposure typical of the tumor milieu.
Professor Alfred Zippelius and his research team performed extensive ex vivo analyses on immune cells isolated from lung cancer patients, revealing that their fusion protein stimulates a multifaceted immune response. These activated immune cells demonstrated increased cytotoxic capability, directly engaging and destroying tumor cells. Strikingly, the therapy avoided the activation of regulatory T cells, which can otherwise undermine antitumor activity by enforcing immunosuppression. The study’s findings illuminate a crucial balance—this fusion molecule not only frees immune cells from exhaustion but also ensures their selective activation, fostering a robust immune assault within the tumor normalized to the patient’s own immunological landscape.
The research utilized sophisticated immunological assays to delineate the molecular and cellular responses induced by the fusion protein. Flow cytometry and single-cell RNA sequencing were employed to characterize the phenotypic changes in tumor-infiltrating lymphocytes pre- and post-treatment. The data confirmed reinvigoration of CD8+ effector T cells and NK populations, with increased expression of cytotoxic granules and pro-inflammatory cytokines—a hallmark of effective immune-mediated tumor killing. Meanwhile, suppressive phenotypes remained unaltered, highlighting the selective nature of this approach. Such precision provides a blueprint for minimizing the systemic toxicities that plagued earlier IL-2 therapies.
The fusion of PD-1 blockade with IL-2 variant delivery represents a sophisticated example of combining immune checkpoint inhibition with cytokine therapy, both of which have been transformative in oncology but with limitations when used independently. Immune checkpoint inhibitors targeting PD-1 or its ligand PD-L1 have revolutionized cancer treatment by unleashing antitumor immunity, yet their efficacy remains limited in many patients due to immune exhaustion and an immunosuppressive microenvironment. Traditional IL-2 therapies, while broadly immunostimulatory, often triggered disproportionate immune activation and off-target toxicity. This fusion strategy elegantly unites these elements to overcome both hurdles simultaneously.
From a mechanistic perspective, the fusion protein works by adhering selectively to PD-1 on exhausted T cells within the tumor, acting as a homing mechanism. This precise targeting ensures that the IL-2 variant achieves localized activation of these impaired effector cells, restoring their functionality and proliferative capacity. At the same time, by interrupting PD-1 mediated inhibitory signals, the fusion molecule directly counteracts tumor-mediated immunosuppression. The coordinated cis-delivery thus initiates a synergistic cascade: T cells reawaken, proliferate, and mount sustained cytotoxic responses, ultimately leading to heightened tumor destruction.
The therapeutic potential of this modality extends beyond lung cancer, with possible applications across various solid tumors characterized by immune evasion strategies centered on PD-1/PD-L1 pathways and T cell exhaustion. By refining both specificity and activity, the fusion protein represents a versatile immunotherapeutic platform capable of personalizing treatment to the patient’s tumor immunophenotype. Further clinical development is underway, with a phase I trial currently enrolling patients to assess safety, optimal dosing, and preliminary efficacy in a clinical setting, spearheaded by Roche.
The implications of this research extend deeply into the broader field of cancer immunotherapy. It addresses a longstanding challenge: how to invigorate anti-cancer immune responses robustly, yet safely, without precipitating the severe immune-related adverse events that have curtailed the utility of some powerful immunotherapies. By selectively targeting and rescuing the tumor-killing arms of the immune system and mitigating inhibitory signals, this fusion protein strategy ushers in a new era of precision immunotherapy, potentially raising survival rates while enhancing patient quality of life.
Moreover, the study underscores the power of multidisciplinary collaboration—melding molecular engineering, immunology, and clinical oncology—to innovate transformative therapies. The University of Basel research team’s successful demonstration of this fusion protein’s efficacy in patient-derived tumor models exemplifies the critical translational bridge from bench to bedside. It sets a compelling precedent for future drug development efforts aiming to overcome immune resistance mechanisms that tumors deploy.
In sum, the conception and validation of this PD-1-targeted IL-2 variant fusion protein delineate a promising therapeutic frontier—one that not only reawakens the immune system’s intrinsic tumor-fighting capabilities but also circumvents previous obstacles associated with conventional immunotherapies. As phase I clinical trials progress, the oncology community eagerly anticipates whether this fusion approach will herald a new standard of care, offering renewed hope to patients confronted with otherwise intractable malignancies.
Subject of Research: Cancer immunotherapy combining PD-1 checkpoint blockade with IL-2 variant delivery in lung cancer
Article Title: PD1-targeted cis-delivery of an IL-2 variant induces a multifaceted anti-tumoral T cell response in human lung cancer
News Publication Date: 17-Sep-2025
Web References: DOI: 10.1126/scitranslmed.adr3718
Image Credits: M. Oeggerli (Micronaut 2019), Marcel Philipp Trefny, and Prof. Alfred Zippelius, Translational Oncology, University Hospital Basel, supported by Pathology University Hospital Basel, and C-CINA, Biozentrum, University of Basel
Keywords: immunotherapy, cancer, IL-2 variant, PD-1, immune checkpoint blockade, lung cancer, T cell exhaustion, fusion protein, tumor microenvironment, immune activation