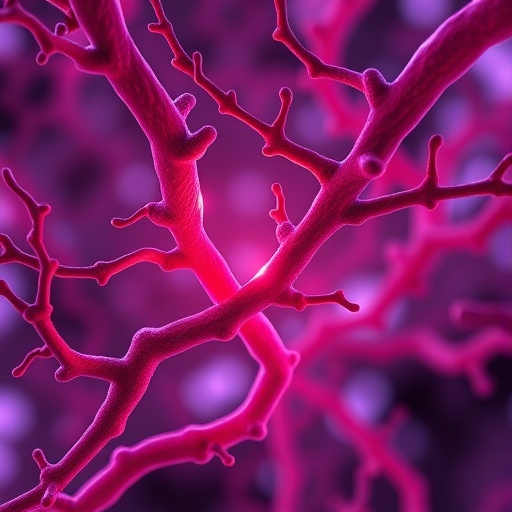
A newly uncovered natural regulator of vascular integrity, heparanase 2 (Hpa2), has emerged as a promising molecule capable of safeguarding blood vessel health and potentially transforming therapies for a multitude of vascular-related diseases. Spearheaded by Dr. Hermann Haller, President of MDI Biological Laboratory, and postdoctoral researcher Yannic Becker, Ph.D., this groundbreaking discovery elucidates how Hpa2 functions at the molecular level to maintain the structural and functional stability of the endothelium, the delicate cellular lining of blood vessels responsible for controlling permeability and molecular exchange.
The vascular system’s integrity is crucial to overall health, as dysfunction in blood vessels underlies numerous pathological states including cardiovascular disease, chronic kidney disease, vision impairment, and cancer progression. Traditionally, therapies have aimed to modulate growth factor signaling pathways, particularly those involving vascular endothelial growth factor (VEGF), which is instrumental in angiogenesis and endothelial cell regulation. However, unrestrained VEGF activity often triggers excessive vascular permeability, leading to leaky vessels and conditions such as diabetic retinopathy and proteinuria. This new research offers compelling evidence that Hpa2 naturally inhibits overactive VEGF signaling, thus preserving vascular homeostasis.
Hpa2 is a relatively obscure molecule until now, but the team’s experimental studies using zebrafish, murine kidney models, and human endothelial cell cultures revealed its vital role in vascular biology. Unlike its close relative heparanase 1, which is known for its enzymatic degradation of heparan sulfate proteoglycans (HSPGs), Hpa2 competes non-enzymatically with VEGF and other growth factors for binding sites on the endothelial cell surface. This competition effectively dampens excessive growth factor-induced signaling without degrading the crucial HSPGs, thereby maintaining the structural scaffold necessary for endothelial function.
Mechanistically, the endothelium’s permeability depends heavily on the interaction between heparan sulfate chains and signaling molecules anchored at the cell surface. These sugar-rich proteoglycans act as gatekeepers, mediating signaling cascades that dictate cell behavior—proliferation, migration, and barrier function. Hpa2 binds strongly to these same heparan sulfate sites, modulating the access and intensity of growth factor engagement. This regulatory action ensures the endothelial barrier remains selectively permeable, preventing pathological leakage of plasma components into surrounding tissues.
In a striking revelation, the absence or genetic knockdown of Hpa2 in zebrafish models resulted in significant disruption of endothelial cell architecture and a marked increase in vascular permeability. This leaky vasculature phenotype mirrors clinical pathologies characterized by compromised vessel integrity, underscoring Hpa2’s indispensable function. More importantly, administration of recombinant Hpa2 protein in mouse kidney tissues successfully restored normal vascular permeability and countered VEGF-driven endothelial dysfunction, demonstrating a potent therapeutic potential.
Hpa2’s mode of action stands apart from conventional VEGF inhibitors, which broadly suppress growth factor signaling but often cause undesirable side effects by interfering with physiological angiogenesis necessary for tissue repair and maintenance. By selectively competing for heparan sulfate binding without complete blockade, Hpa2 appears to fine-tune signaling dynamics, offering a nuanced approach to vascular stabilization. This precision could make Hpa2-based interventions more effective and better tolerated than current pharmacological options.
The team’s multidisciplinary approach combined advanced molecular biology techniques, in vivo functional assays, and biochemical binding studies to paint a comprehensive picture of Hpa2’s role. Zebrafish models provided an ideal in vivo platform due to their transparent vasculature and genetic tractability, enabling real-time visualization of vascular defects. Complementary experiments in mouse kidney tissue confirmed translational relevance, while human endothelial cell cultures allowed for detailed mechanistic dissection at the cellular level.
Beyond vascular diseases, these findings hold implications for oncology, where tumor angiogenesis hijacks blood vessels to sustain malignant growth. By restoring vascular integrity and regulating permeability, Hpa2 could impede tumor vasculature exploitation, representing a promising adjunct to current anti-cancer strategies. Moreover, its natural occurrence across vertebrates suggests evolutionary conservation and an inherent safety profile, increasing enthusiasm for therapeutic development.
Despite these exciting advances, considerable challenges remain before Hpa2 can transition from bench to bedside. Detailed pharmacokinetic profiling, long-term safety evaluation, and clinical efficacy studies will be essential to harnessing Hpa2 as a viable drug candidate. Nevertheless, the discovery underscores an expanding paradigm shift in biomedical research: leveraging endogenous molecules to restore physiological balance rather than solely blocking pathological pathways.
In a broader context, this research highlights the critical importance of extracellular matrix components like heparan sulfate in regulating intercellular communication and vascular biology. The interplay between proteoglycans and growth factors is complex and delicate, and molecules such as Hpa2 serve as critical modulators within this system. Understanding such interactions enhances our grasp of vascular homeostasis and devises novel avenues for clinically addressing widespread disorders involving endothelial dysfunction.
Dr. Becker emphasized the transformative potential of their findings, noting, “Our identification of heparanase 2 as a natural guardian of vascular integrity challenges traditional views and opens new horizons for non-toxic, biologically attuned therapies. The ability to restore barrier function without impairing essential growth signaling is a significant step forward.” This sentiment is echoed by Dr. Haller, who envisions that Hpa2-based therapies may complement or even surpass current modalities, offering hope to millions suffering from chronic vascular conditions.
Collectively, this work provides a compelling blueprint for future research targeting vascular permeability regulation. It points to the therapeutic promise of fine-tuned modulation of growth factor interactions using endogenous molecular players, fostering a more natural, balanced approach to treating disorders rooted in endothelial barrier dysfunction. As knowledge expands, Hpa2 may well become a cornerstone molecule in vascular medicine, redefining how we conceptualize and manage the delicate architecture of blood vessels worldwide.
Subject of Research: Animal tissue samples
Article Title: Heparanase 2 Modulates Vascular Permeability via Heparan Sulfate–Dependent Growth Factor Signaling
News Publication Date: September 2, 2025
Web References: https://www.ahajournals.org/doi/epub/10.1161/ATVBAHA.125.323060
References: Arteriosclerosis, Thrombosis, and Vascular Biology, DOI: 10.1161/ATVBAHA.125.323060
Keywords: Health and medicine, Diseases and disorders, Human health, Biomedical engineering