In the relentless pursuit of understanding the molecular drivers behind endometrial cancer, a recent study has spotlighted XPR1 as a promising new prognostic indicator. This revelation comes at a critical time when identifying biomarkers that can reliably predict patient outcomes remains a foremost challenge for oncologists and researchers alike. The comprehensive analysis of XPR1 expression and its biological implications in endometrial carcinoma not only expands our molecular grasp of this malignancy but also hints at untouched therapeutic avenues that may transform patient management strategies in the near future.
Endometrial cancer (EC), one of the most prevalent gynecologic malignancies worldwide, has historically suffered from a paucity of robust biomarkers that accurately reflect tumor aggressiveness and patient prognosis. XPR1, known scientifically as Xenotropic and Polytropic Retrovirus Receptor 1, traditionally linked to retroviral entry mechanisms, emerges here with a far more sinister profile — one intimately connected to tumor progression and immune microenvironment modulation. The study in question leverages cutting-edge bioinformatics alongside rigorous cellular experimentation to unravel the multifaceted role of XPR1 within the endometrial tumor landscape.
The researchers embarked on their investigation by mining the extensive dataset of The Cancer Genome Atlas (TCGA), focusing on 554 cases of Uterine Corpus Endometrial Carcinoma (UCEC) alongside 35 normal endometrial tissue controls. The bioinformatics sieving revealed a marked overexpression of XPR1 in cancerous tissues, with statistical robustness indicating a significant deviation from healthy counterparts. This differential expression hinted strongly at a potential role for XPR1 not merely as a passenger in tumor biology but as an active contributor to carcinogenesis.
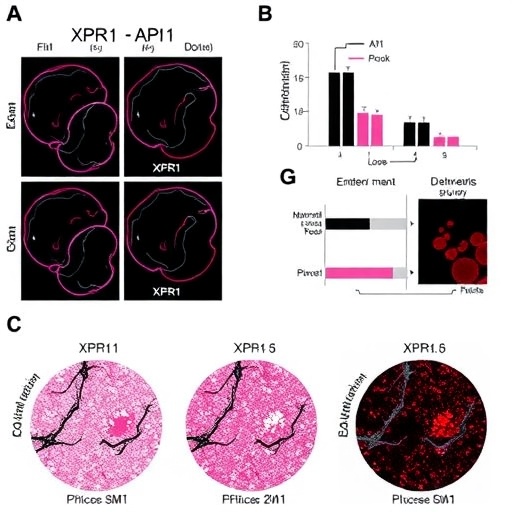
Validating these computational findings, Western blot analyses were conducted on established EC cell lines (ECC-1) and normal endometrial cells (EEC), confirming that XPR1 protein levels were notably elevated in malignant cells. This protein-level confirmation bridges the critical gap between gene expression and functional protein presence, an essential criterion for biomarker viability. It also laid the groundwork for functional assays probing the direct consequences of XPR1 modulation on cancer cell behavior.
Functionality tests incorporated EdU proliferation assays and Transwell invasion experiments, compellingly demonstrating that heightened XPR1 expression confers increased proliferative and invasive capabilities to EC cells. These phenotypic changes resonate with aggressive tumor characteristics, suggesting that XPR1 overexpression equips cancer cells with enhanced mechanisms to thrive and metastasize. In parallel, analyses revealed correlations between XPR1 levels and key clinical parameters such as patient age, body mass index (BMI), tumor stage, histological grade, and invasiveness—parameters routinely used in clinical settings for risk stratification.
A particularly intriguing dimension of this study delves into the epitranscriptomic landscape, centering on m6A methylation—a dynamic and reversible RNA modification influencing post-transcriptional gene expression. Utilizing Dot blot assays, researchers observed that XPR1 overexpression is accompanied by elevated m6A methylation levels in EC cells compared to normal controls. Moreover, correlations between XPR1 and multiple m6A-related regulatory genes were identified through sophisticated computational analyses. While the evidence stops short of confirming a direct regulatory role of XPR1 on m6A modification, the association underscores a potentially critical axis that might modulate tumor biology through post-transcriptional mechanisms.
Equally compelling are the findings regarding the tumor immune microenvironment. The study employed immune cell infiltration analyses revealing significant associations between XPR1 expression and the presence of various immune cell subsets, including B cells, CD4+ and CD8+ T lymphocytes, macrophages, neutrophils, and dendritic cells. This suggests that XPR1 might influence oncogenic processes not only via direct cellular proliferation but also by orchestrating immune interactions within the tumor niche. Such immune-tumor cross-talk is a rapidly evolving area of study with vast implications for immunotherapy responsiveness and resistance mechanisms.
Clinically, the prognostic value of XPR1 was interrogated through Kaplan–Meier survival curves and Cox regression analyses. Patients exhibiting high XPR1 expression presented significantly reduced overall survival rates. The hazard ratio indicated a 60% increased risk of mortality compared to low-expression counterparts, firmly positioning XPR1 as a marker of poor prognosis. However, multivariate analyses tempered these conclusions by failing to establish XPR1 as an independent prognostic factor when adjusted for other clinical variables. This nuance emphasizes the complexity of cancer prognostication and the need for multi-parametric models incorporating XPR1 alongside traditional markers.
To address this complexity, the team devised a novel prognostic nomogram integrating XPR1 expression with clinical stage and other patient-specific factors to predict survival probabilities at 1, 3, and 5 years post-diagnosis. Calibration curves demonstrated robust predictive accuracy, suggesting that incorporating XPR1 into prognostic frameworks could enhance clinical decision-making and patient counseling. However, the authors prudently acknowledge that further validation in diverse cohorts will be essential before this model can see widespread adoption.
On the molecular front, gene ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses illuminated that genes co-expressed with XPR1 are enriched in pathways governing RNA processing, DNA metabolism, and key signaling cascades implicated in cancer progression. These enriched pathways provide fertile ground for future mechanistic studies and potential therapeutic targeting, particularly if XPR1’s role extends into modulating the epigenetic and epitranscriptomic landscape.
Despite the promising findings, significant questions remain unanswered, particularly regarding the mechanistic underpinnings of XPR1’s interactions with m6A methylation machinery. The absence of direct evidence for XPR1-mediated regulation of m6A suggests a need for further molecular dissection, potentially involving CRISPR-Cas9-mediated gene editing or RNA immunoprecipitation sequencing (RIP-seq) to delineate binding partners and downstream targets. Such deepened insights will be critical to move from correlative observations to mechanistic causality that can inform drug development.
The study also raises the possibility that XPR1 could serve as a therapeutic target, especially if its influence on proliferation, invasion, and immune modulation proves druggable. Given the expanding array of small molecules and monoclonal antibodies directed against cell surface receptors, XPR1’s known receptor status confers tangible potential for pharmacological intervention. Nevertheless, the complexity of its involvement in essential biological pathways mandates carefully designed investigations to avoid unforeseen toxicities.
Importantly, this work underscores the broader thematic shift in oncology towards integrating multiple omics layers—genomic, transcriptomic, and epitranscriptomic—to capture the heterogeneous nature of cancer. The identification of XPR1 as a nexus linking gene expression, RNA modifications, and immune milieu exemplifies this integrated approach, highlighting the necessity for transdisciplinary research strategies that marry bioinformatics with wet-lab validation.
As the global burden of endometrial cancer escalates, especially in aging and obese populations, the urgency to refine prognostic classifiers and identify actionable biomarkers intensifies. This research represents a step forward, illuminating the complex interplay of factors driving disease progression and exposing XPR1 as a multifaceted player in tumor biology. Its prospective utility as both a prognostic indicator and a molecular target bears promise for personalized therapies tailored to molecular tumor profiles.
Moving forward, prospective clinical studies assessing XPR1 expression in patient biopsies, alongside immune profiling and epitranscriptomic analyses, will be essential. These efforts should aim not only to validate the prognostic relevance but also to evaluate therapeutic implications, such as responsiveness to immune checkpoint inhibitors or epigenetic modulators. Additionally, patient-derived xenograft and organoid models could provide critical experimental platforms to explore the functional ramifications of XPR1 silencing or overexpression in a physiologically relevant setting.
In conclusion, this landmark study deepens the scientific community’s understanding of the molecular intricacies characterizing endometrial cancer. By illuminating the prognostic significance of XPR1 and its associations with m6A methylation and immune infiltration, it provides a compelling impetus for further exploration. While challenges remain in establishing causality and therapeutic feasibility, the findings herald a new chapter in the quest to conquer one of women’s most common and deadly cancers.
Subject of Research:
XPR1 as a prognostic biomarker and its role in proliferation, invasion, m6A RNA methylation, and immune infiltration in endometrial cancer.
Article Title:
In-depth evaluation of XPR1 as a new prognostic indicator for endometrial cancer
Article References:
Han, X., Yang, L., Nuermanguli, R. et al. In-depth evaluation of XPR1 as a new prognostic indicator for endometrial cancer. BMC Cancer 25, 1411 (2025). https://doi.org/10.1186/s12885-025-14818-1
Image Credits:
Scienmag.com