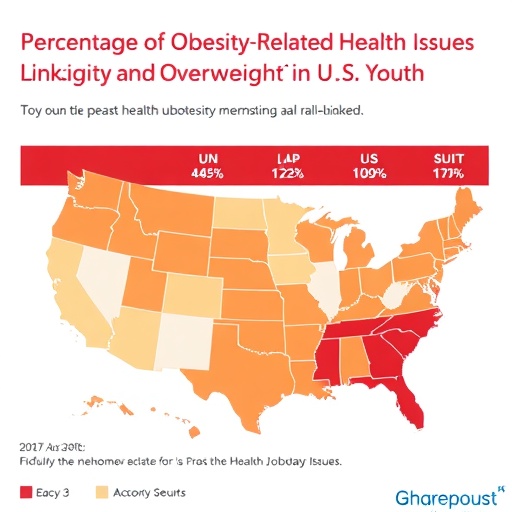
A recent landmark study published in JAMA Pediatrics highlights the profound impact of obesity on health outcomes among U.S. adolescents and young adults. This research reveals that a significant proportion of obesity-related medical conditions in this population can be directly attributed to obesity itself, with overweight status also contributing to a lesser, yet meaningful extent. As the prevalence of obesity climbs among younger demographics, understanding its long-term health implications becomes increasingly critical for both clinical and public health interventions.
The study meticulously quantifies the burden of obesity-related diseases during youth, underscoring how these early-life health challenges predispose individuals to more severe, chronic complications in adulthood. This developmental trajectory accentuates the necessity for early preventive measures and effective treatment strategies to curtail the progression of disease and mitigate future healthcare demands. The research team employed rigorous epidemiological methods to estimate the population-attributable risk of numerous metabolic and cardiovascular conditions linked to excessive body weight.
One particularly striking finding of the study is the identification of obesity as a principal modifiable risk factor for the emergence of metabolic disorders such as Type 2 diabetes and dyslipidemia in adolescents and young adults. These conditions not only compromise immediate health but also set the stage for persistent multimorbidity and premature mortality. The mechanistic underpinnings involve complex interactions between adipose tissue dysfunction, systemic inflammation, and insulin resistance that accelerate disease pathogenesis.
Moreover, the researchers examined the economic consequences associated with obesity-related morbidity in youth, revealing substantial healthcare costs stemming from increased utilization of medical services, pharmacotherapy, and hospitalizations. These findings illuminate the immense financial burden borne by the United States healthcare system and highlight the urgent need for cost-effective interventions that address weight management in early life stages.
Importantly, the study sheds light on the differential impacts of overweight and obesity, clarifying that while overweight status independently elevates risk for certain conditions, the magnitude of risk associated with obesity is considerably greater. This distinction offers crucial insight for tailored public health messaging and clinical prioritization, as interventions must be calibrated to address varying degrees of excess weight and related health risks.
The investigative team also acknowledges the multifactorial nature of obesity, pointing out how social determinants of health—including socioeconomic status, environmental factors, and access to healthcare—intersect with biological susceptibility to influence disease trajectories. This multidimensional perspective is vital for developing holistic strategies that incorporate preventive medicine alongside broader social policies aimed at reducing disparities.
From a preventive medicine standpoint, the study reinforces the importance of early detection and intervention programs targeting children and adolescents. Lifestyle modifications encompassing improved nutrition, increased physical activity, and behavioral counseling serve as cornerstone strategies in this endeavor. When these measures fail or prove insufficient, clinical treatments, including pharmacological agents or bariatric procedures, may be necessary to achieve meaningful weight reduction and attenuate disease risk.
The study’s findings also bring into focus the pediatric healthcare domain, emphasizing that pediatricians and adolescent medicine specialists play a pivotal role in identifying at-risk individuals and orchestrating multidisciplinary care models. Through proactive screening and patient-centered counseling, healthcare providers can intervene at critical junctures, potentially reversing or slowing the course of obesity-related pathology before irreversible damage ensues.
Given the public health ramifications, policymakers and stakeholders are encouraged to prioritize funding and resources for research and programs that address childhood and young adult obesity. The compelling evidence from this study provides a data-driven rationale for expanding preventive services and education, particularly within underserved communities that experience disproportionate burdens of obesity and associated diseases.
In summary, this comprehensive study elucidates the substantial contribution of obesity and overweight to early-onset metabolic and cardiovascular diseases among U.S. youth. The findings underscore an urgent call to action: an integrated approach involving clinical care, public health initiatives, and social policy reforms is imperative to stem the tide of obesity-related morbidity and the associated economic strain. Such an approach promises not only enhanced quality of life for affected individuals but also sustainable healthcare systems equipped to handle future challenges.
As the obesity epidemic continues to evolve, the insights derived from this landmark study pave the way for innovative research and intervention paradigms. By understanding the biological, social, and economic complexities of obesity in early life stages, the medical community can better tailor strategies that offer hope for a healthier future generation free from the disabling sequelae of excess weight.
For the healthcare sector, the implications are far-reaching. Investment in early prevention and treatment now will likely yield dividends in reducing the incidence of adult chronic diseases, thereby alleviating long-term medical costs and enhancing population health metrics. This study significantly advances the knowledge base, making a compelling case for immediate and sustained commitment to combating obesity from adolescence onward.
Subject of Research: Impact of obesity and overweight on obesity-related conditions in U.S. adolescents and young adults
Article Title: Not available
News Publication Date: Not available
Web References: Not available
References: (doi:10.1001/jamapediatrics.2025.2716)
Image Credits: Not available
Keywords: Obesity, Young people, United States population, Adults, Health care costs, Risk factors, Preventive medicine, Adolescents, Disease prevention, Weight gain, Pediatrics