An unprecedented two-decade analysis of suicide rates across England has revealed complex and often surprising links between local socio-environmental factors and regional suicide risks. Spearheaded by researchers from Imperial College London in collaboration with University College London (UCL) and the London School of Economics and Political Science (LSE), this extensive study connects the spatial and temporal dynamics of suicide mortality with a range of environmental indicators. It highlights not only entrenched social inequalities but uncovers nuanced relationships with infrastructure and ecological attributes that may redefine suicide prevention efforts.
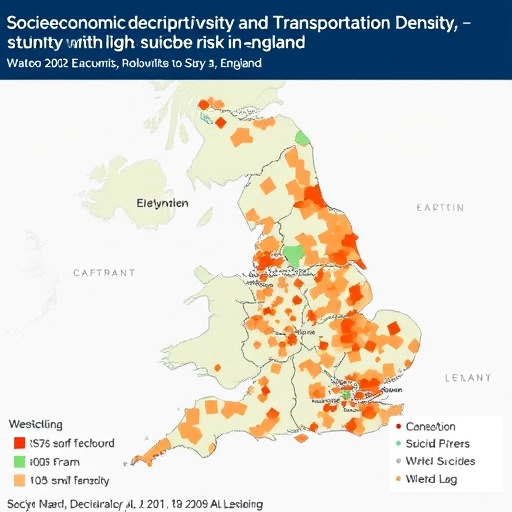
Covering the years 2002 through 2022, the researchers aggregated and methodically analyzed mortality data sourced from the Office for National Statistics (ONS), spanning nearly 7,000 administrative zones in England. Each area, averaging populations of around 15,000, was examined for suicide death counts, mapped against variables such as social deprivation indices, ethnic composition, population density, and environmental parameters including light pollution, green spaces, and transport network densities. What emerged was a multifaceted and geographically heterogeneous picture of suicide risk across the country.
On a national level, the overall suicide rate in England has remained surprisingly consistent over the 20-year period, averaging approximately 11 deaths per 100,000 people annually. Despite this apparent stability, the researchers observed significant fluctuations in year-to-year relative risk, dipping especially low in 2007 before peaking in 2019. Regional disparities were even more striking. The North East, for example, exhibited suicide rates more than 14% above the national average, while London consistently recorded rates nearly 18% lower, underscoring a stark north-south divide with nearly 40% difference between the highest and lowest risk regions.
Delving into socio-environmental determinants, the study employed advanced ecological modeling techniques to quantify how unit changes in local factors corresponded to shifts in suicide risk. Unsurprisingly, higher social deprivation—a composite measure capturing economic hardship, limited services, and unemployment—was strongly correlated with increased risk, elevating suicide rates by around 20% per standard deviation increase. However, the study also identified critical roles for physical infrastructure: greater density of roads and railways were independently linked with modest but significant boosts in suicide risk, by 5.16% and 1.37% respectively.
Conversely, certain urban characteristics appeared protective. Higher ethnic diversity and population density correlated with lower suicide risk, decreasing it by approximately 7.5% and 5.4% per standardized increment. Similarly, areas with more extensive green space coverage and higher levels of ambient light pollution showed diminished suicide risk, challenging some conventional assumptions. The protective association with light pollution is particularly intriguing, potentially reflecting greater urbanization and social connectivity, though it invites further mechanistic investigation.
Experts emphasize that while individual suicide risk factors are complex and multifactorial—encompassing mental health conditions, substance use, and personal circumstances—this study illuminates the profound influence of place and community context. Spatial disparities indicate that where someone lives can significantly affect their suicide risk, mediated by economic, demographic, and environmental variables. This ecological perspective complements established clinical knowledge, offering new avenues for targeted intervention.
The research underscores how transport infrastructure might influence suicide risk through multiple pathways. Roadways and railway networks may facilitate access to lethal means, segment communities, and contribute to environmental stressors such as noise and air pollution. Conversely, they might also represent social connectivity avenues that promote mental well-being. Decoding these complex mechanisms is a crucial priority, potentially informing urban planning and public health policy to mitigate unintended harms.
Similarly, the findings on ethnic density align with broader literature recognizing the protective social cohesion and cultural support often found in ethnically diverse communities. This dynamic may bolster resilience against social isolation and its deleterious mental health consequences. The inverse relationship between green space and suicide risk reinforces emerging evidence that access to natural environments supports mental health by reducing stress and promoting physical activity.
Despite its comprehensive scope, the study acknowledges limitations inherent to ecological designs. The absence of individual-level data on variables such as ethnicity, family status, employment, and socioeconomic position constrains causal interpretations. Moreover, the lack of detail on suicide methods prevents assessment of how environmental factors may differentially influence means selection. The exclusive focus on England limits generalizability to other UK nations or internationally.
The implications of these findings reverberate through current public health frameworks. They dovetail with the NHS’s recently published 10-Year Health Plan, which prioritizes suicide prevention alongside early intervention strategies. By enabling the mapping of high-risk locales and tracking temporal changes in risk factors, this research introduces novel data-driven tools to complement traditional mental health services. Such localized approaches could optimize resource allocation and enhance the effectiveness of prevention programs.
Stakeholders beyond academia have voiced support for these insights. Mental health authorities lament ongoing regional inequalities and underscore the necessity of channeling funding and services to historically underserved communities, particularly in the North East and North West of England. The study’s granular revelations provide a robust empirical foundation to advocate for such policy realignments, encouraging a shift from anecdotal observations to evidence-based action.
Further interdisciplinary collaboration is essential to unlock the mechanisms through which environmental and infrastructural factors modulate suicide risk. This includes leveraging geospatial analytics, urban design expertise, and behavioral science to develop integrated interventions. By doing so, society may diminish the stark regional disparities in suicide rates and alleviate the burden borne disproportionately by deprived and isolated populations.
Ultimately, this landmark study not only advances scientific understanding of suicide epidemiology but also offers a pragmatic blueprint for policymakers, public health professionals, and community leaders. Recognizing that suicide rates are not static nor uniform but dynamically influenced by environmental and social factors is a clarion call to innovate prevention efforts. Through informed, place-sensitive strategies, the goal of reducing suicide and promoting mental health equity across England can become progressively attainable.
Subject of Research: People
Article Title: Spatio-temporal trends and socio-environmental determinants of suicides in England (2002 – 2022): an ecological population-based study
News Publication Date: 14-Aug-2025
Web References: http://dx.doi.org/10.1016/j.lanepe.2025.101386
References:
- National Confidential Inquiry into Suicide and Safety in Mental Health. Annual Report: UK patient and general population data 2011-2021, University of Manchester, 2024.
- Suicide statistics, Commons Library Research Briefing, 8 January 2025, by Esme Kirk-Wade.
- ‘Fit for the Future: 10 Year Health Plan for England’, NHS England, 2025.
Keywords:
Public policy, suicide epidemiology, social deprivation, environmental health, transport infrastructure, mental health, spatial epidemiology, population health, urban planning, health inequalities, suicide prevention, socio-environmental determinants