In a groundbreaking new study published in Schizophrenia (2025), researchers have unveiled compelling evidence linking glymphatic system dysfunction to gut microbiome imbalance and cognitive deficits in individuals diagnosed with schizophrenia. This integrative research sheds light on the intricate interplay between brain clearance pathways, microbial ecology within the gut, and the manifestations of impaired cognitive function frequently observed in this complex psychiatric disorder. By unraveling these associations, the study pushes forward a paradigm shift in understanding schizophrenia beyond a purely neurochemical or neurodevelopmental disorder, positioning it within a broader systemic context involving neuroimmune and neurovascular components influenced heavily by microbiota homeostasis.
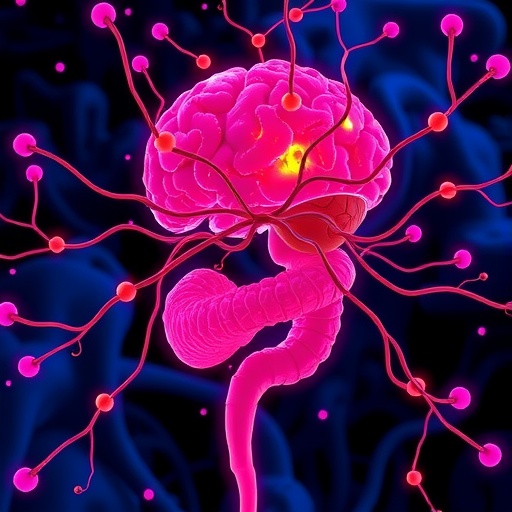
The glymphatic system is a relatively recently characterized brain-wide perivascular network responsible for the clearance of metabolic waste and neurotoxic proteins from the central nervous system. Operational primarily during sleep, it facilitates cerebrospinal fluid (CSF) influx alongside interstitial fluid flow, effectively washing away harmful solutes. Dysregulation of this clearance mechanism has been implicated in neurodegenerative disorders such as Alzheimer’s disease and chronic traumatic encephalopathy, but its role in psychiatric illnesses like schizophrenia has remained understudied until now. This study distinctly positions glymphatic dysfunction as a putative contributor to the cognitive impairments characteristic of schizophrenia, suggesting a novel biomarker and potential therapeutic target.
What is particularly innovative about this research is the integration of gut dysbiosis — an imbalance in the complex microbial community inhabiting the gastrointestinal tract — into the pathophysiological framework of glymphatic system impairment. The human gut microbiome has gained significant attention in recent years for its modulatory influence on brain function via the gut-brain axis, a multifaceted communication route involving neural, immune, endocrine, and metabolic pathways. Alterations in gut microbiota composition have previously been linked to schizophrenia, but the mechanistic pathways underlying these associations were ambiguous. This study bridges that gap by linking gut dysbiosis directly with compromised brain clearance capacity.
Employing multimodal imaging techniques, including advanced MRI sequences capable of assessing glymphatic transport efficiency, alongside comprehensive gut microbiota profiling via 16S rRNA gene sequencing, the authors meticulously correlated biomarkers indicative of glymphatic impairment with microbial community structure anomalies in a large cohort of schizophrenia patients. These measurements were then cross-examined against cognitive performance metrics—particularly focusing on domains such as working memory, executive control, and processing speed, which are commonly disrupted in schizophrenia.
The data reveal that individuals with schizophrenia exhibit significant reductions in glymphatic clearance capacity compared to healthy controls, accompanied by marked shifts in gut microbiome diversity and composition. Notably, the abundance of beneficial microbial taxa known for anti-inflammatory and neuroprotective functions, such as Lactobacillus and Bifidobacterium, were depleted, while opportunistic and pro-inflammatory bacteria were enriched. This gut dysbiosis correlated strongly with impaired glymphatic function and, importantly, poorer cognitive testing outcomes, delineating a trajectory of systemic dysfunction manifesting in neuropsychiatric symptoms.
Neuroinflammation emerges as a pivotal mediator within this complex triad. The study explores how microbial-derived metabolites and endotoxins penetrate systemic circulation due to a compromised intestinal barrier — a phenomenon often observed in schizophrenia — triggering systemic immune activation. This chronic low-grade inflammation may then impact the integrity of perivascular astrocytic endfeet and aquaporin-4 water channels critical for glymphatic flow, resulting in diminished clearance of metabolic byproducts. The accumulation of such toxic protein aggregates and inflammatory mediators within the CNS milieu is hypothesized to exacerbate synaptic dysregulation and neural network dysfunction, thereby accounting for cognitive deficits.
Moreover, sleep disruption—highly prevalent among patients with schizophrenia—is considered both a cause and consequence of glymphatic dysfunction. Given that glymphatic clearance is most efficient during slow-wave sleep, alterations in sleep architecture can diminish waste removal efficiency, creating a vicious cycle that amplifies neurocognitive impairment. The study posits that gut microbiota alterations could also influence sleep quality via microbial production of neuroactive compounds such as serotonin precursors, further entangling the gut-brain dialogue in this pathology.
These findings advocate for a revision of current therapeutic strategies, emphasizing the potential of microbiome-targeted interventions to restore glymphatic function and ameliorate cognitive symptoms. Approaches including probiotic supplementation, dietary modification, prebiotics, and even fecal microbiota transplantation might feasibly rebalance gut dysbiosis. In parallel, emerging treatments aimed at modulating aquaporin-4 expression or enhancing perivascular flow could synergistically restore brain clearance mechanisms.
The translational implications are vast. Detecting glymphatic dysfunction non-invasively offers a promising biomarker for early diagnosis, disease staging, and therapeutic monitoring in schizophrenia. Furthermore, personalized medicine approaches integrating microbiome profiling and glymphatic imaging could pave the way for individualized treatment paradigms, moving psychiatry towards a more precision-based discipline.
Importantly, this study also raises fundamental neuroscientific questions about the bidirectional influence between gut microbes and cerebral homeostasis. It challenges the traditional compartmentalization within neuroscience and psychiatry, advocating for integrative models that incorporate peripheral systems as active participants in neuropsychiatric disease mechanisms.
However, the study acknowledges limitations including its cross-sectional design, which precludes definitive causal inference. Longitudinal studies and controlled interventions are needed to ascertain if modifying gut microbiota composition can directly enhance glymphatic function and improve cognitive outcomes. Additionally, expanding sample sizes and diverse populations will be critical to generalize findings and unravel demographic or genetic moderators.
Future research directions may explore the molecular mediators linking gut microbial metabolites with astrocytic function and perivascular dynamics in the brain. Advanced in vivo imaging combined with metabolomic and transcriptomic analyses will be invaluable in dissecting these pathways. Animal models engineered for targeted microbiome manipulation and glymphatic monitoring could also elucidate mechanistic underpinnings and facilitate preclinical therapeutic trials.
In summary, this trailblazing work by Wu and colleagues orchestrates an unprecedented convergence of neuroimaging, microbiology, immunology, and cognitive neuroscience to elucidate a systemic basis for schizophrenia’s cognitive impairments. By illuminating the nexus between glymphatic system dysfunction and gut dysbiosis, it not only expands the biological landscape of schizophrenia but also heralds novel diagnostic and therapeutic horizons. Such integrative insights resonate profoundly within an era defined by the pursuit of holistic, multi-dimensional understandings of brain disorders, heralding hope for improved outcomes in a historically treatment-resistant condition.
Subject of Research: Glymphatic system dysfunction, gut microbiome dysbiosis, and cognitive impairment in schizophrenia.
Article Title: Glymphatic system dysfunction correlated with gut dysbiosis and cognitive impairment in schizophrenia.
Article References:
Wu, H., Liu, B., Liu, W.V. et al. Glymphatic system dysfunction correlated with gut dysbiosis and cognitive impairment in schizophrenia. Schizophr 11, 113 (2025). https://doi.org/10.1038/s41537-025-00661-7
Image Credits: AI Generated