In the intricate and devastating realm of oncology, cancer cachexia stands out as one of the most challenging syndromes to understand and manage. Characterized primarily by unintentional weight loss and muscle wasting, this multifactorial condition dramatically worsens quality of life and diminishes survival rates among cancer patients. A recent comprehensive review of clinical trials spanning nearly three decades sheds new light on the evolving research landscape and exposes critical gaps that hamper effective therapeutic advancements.
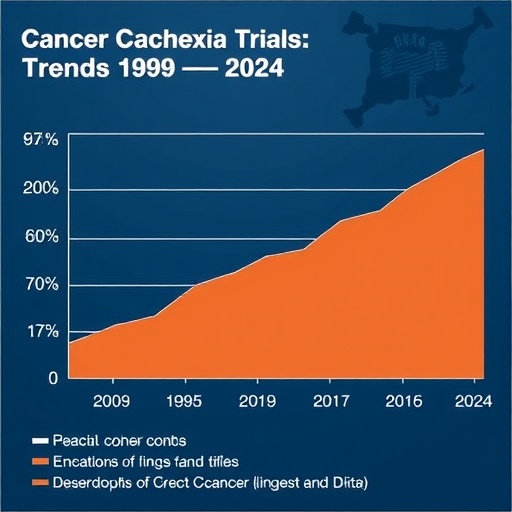
Analyzing data from ClinicalTrials.gov records from 1995 through 2024, researchers have identified significant yet insufficient trends that reflect how clinical studies approach cancer cachexia. Notably, the inclusion of female participants has increased over time, indicating a broader recognition of sex differences in disease manifestation. However, despite this progress, the systematic reporting and analysis of sex as a biological variable remain surprisingly rare, limiting the deep understanding required to tailor interventions effectively.
An even more glaring deficit is revealed in the demographic breakdown of trial participants. Approximately 93% of individuals involved in these clinical trials are of Caucasian descent, exposing a glaring lack of diversity and representation from non-white populations. This lack of inclusivity raises concerns about the generalizability of study results across different ethnic groups, given that genetic and socio-environmental factors heavily influence cachexia’s development and progression.
Adding layers to this complexity is the striking heterogeneity observed in both the diagnosis and measurement of cancer cachexia across studies. Trials employ a vast array of diagnostic criteria and assessment tools, reflecting an absence of standardized protocols or universally accepted definitions. This variability impedes the ability to compare outcomes, synthesize data, or combine findings in meta-analyses, fracturing progress and slowing therapeutic innovation.
The review also underscores a pronounced neglect in considering critical clinical variables such as cancer type and stage. Cachexia does not affect all cancers uniformly; differing tumor biology and disease progression stages significantly influence the syndrome’s onset and severity. Yet, most studies fail to stratify or analyze patients along these lines, missing opportunities to uncover nuanced mechanistic insights or identify subgroup-specific treatment responses.
Such fragmented approaches ultimately contribute to the broader challenge of translating clinical trial results into effective, personalized care for cancer patients suffering from cachexia. While the body of research is undeniably growing, these underreported variables and methodological inconsistencies result in an incomplete picture that risks marginalizing those who do not fit the predominant study profiles, especially non-white individuals and females.
The implications within the broader biological and clinical research communities are profound. With mounting evidence emphasizing human heterogeneity—be it genetic, environmental, or physiological—the cancer cachexia field must evolve beyond a one-size-fits-all mindset. This calls for the urgent development and adoption of consensus definitions and standardized diagnostic and assessment tools that reflect the diverse realities of patient populations worldwide.
Emerging methodologies, including advanced biomarker panels, imaging techniques, and comprehensive phenotyping, offer promising avenues to refine the detection and mechanistic understanding of cachexia. Integrating these novel tools into clinical trial designs could revolutionize patient stratification and enable more accurate monitoring of disease progression and treatment efficacy, addressing long-standing obstacles.
Moreover, the ethical imperative to include diverse populations in clinical research transcends scientific rigor, touching on equity and fairness in healthcare access and outcomes. Enhancing representation ensures that the benefits derived from advances in cachexia management are equitably distributed and that all patient subgroups receive the most appropriate care based on robust evidence.
Parallel to incorporating patient diversity, the recognition of sex as a critical biological variable must become non-negotiable in future studies. Sex-based differences in hormonal milieus, metabolic pathways, and immune responses profoundly affect cachexia’s clinical manifestation. Detailed analyses in this regard could unveil sex-specific therapeutic targets or intervention strategies, improving overall treatment personalization.
By revisiting and updating the cachexia consensus framework regularly, researchers and clinicians can remain aligned with contemporary scientific insights and technological innovations. Such dynamic evolution is essential to keep pace with rapidly accumulating knowledge about cancer biology, systemic inflammation, metabolic dysregulation, and cachexia pathophysiology.
Critically, the current gaps highlighted by this landscape analysis act as a clarion call for multidisciplinary collaboration. Bridging oncologists, nutritionists, physiologists, immunologists, and data scientists will foster holistic approaches that capture the syndrome’s complexity and heterogeneity, facilitating the design of more rigorous and inclusive clinical trials.
Patient advocacy and engagement should also play a central role, as real-world experiences and priorities help guide meaningful endpoint selection and trial design, ensuring that outcomes resonate with patient needs beyond mere biometrics. Incorporating patient-reported outcomes can refine our understanding of cachexia’s impact on quality of life and treatment tolerability.
Ultimately, this retrospective examination of nearly three decades of clinical trials in cancer cachexia underscores both the progress achieved and the considerable work ahead. It reveals a landscape marked by incremental advances but also hampered by methodological disparities and demographic homogeneity, challenging the field to embrace inclusivity and standardization.
The hope is that this reflective review will stimulate the scientific community to heed these recommendations, fostering trials that are not only scientifically robust but also socially equitable. Through such endeavors, the pursuit of effective cachexia therapies can gain renewed momentum, translating into tangible improvements in patient outcomes worldwide.
As cancer continues to threaten millions globally, addressing cachexia with rigor and compassion becomes an ethical and clinical priority. This expansive reassessment stands at the forefront of efforts to reshape research paradigms, catalyze innovation, and ultimately alleviate the heavy burden cachexia imposes on patients and their families.
Subject of Research:
Cancer cachexia and trends in clinical trial design and participant demographics over the period 1995–2024.
Article Title:
Landscape of clinical trials in cancer cachexia: assessment of trends from 1995–2024.
Article References:
Cabrera, A.R., Parker, K., Snoke, D.B. et al. Landscape of clinical trials in cancer cachexia: assessment of trends from 1995–2024. BMC Cancer 25, 1265 (2025). https://doi.org/10.1186/s12885-025-14555-5
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14555-5