In a groundbreaking advance that could reshape the early detection and understanding of psychotic disorders, a new study published in Translational Psychiatry unveils subtle brain texture alterations that precede overt symptoms of psychosis. This research, led by R. Lencer and colleagues, meticulously investigates the microstructural deviations within brain tissue that correlate with visual perceptual dysfunctions in individuals experiencing recent onset psychosis and those identified as being at clinical high risk. Employing cutting-edge neuroimaging techniques combined with sophisticated computational analyses, the study elucidates a previously underappreciated biomarker that holds promise for enhancing diagnostic precision and therapeutic intervention timing in severe mental illnesses.
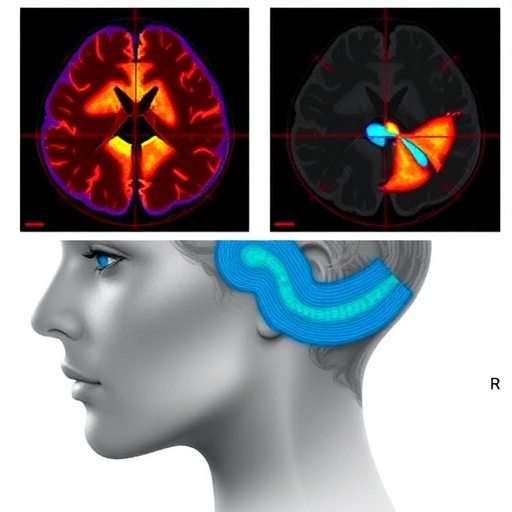
Psychosis typically manifests with pronounced clinical symptoms such as hallucinations, delusions, and impaired cognition, yet these overt signs represent a late stage of a pathological process that often begins months or even years prior. Detecting the neural underpinnings at these prodromal phases remains a critical challenge. The novel approach spearheaded by Lencer’s team leverages advanced brain texture analysis—a sophisticated imaging biomarker technique that captures the heterogeneity of gray matter beyond conventional volumetric assessments. Texture analysis quantifies spatial patterns of pixels or voxels within magnetic resonance imaging (MRI) scans, offering insights into microstructural integrity, organizational complexity, and tissue composition that are invisible to standard MRI metrics.
The researchers recruited a cohort of individuals newly diagnosed with psychosis alongside a group of clinically high-risk participants, encompassing those with attenuated psychotic symptoms or familial predisposition. A comprehensive battery of visual perceptual tasks was administered to assess subtle cognitive and sensory processing deficits, known early manifestations in the trajectory of psychotic disorders. Utilizing high-resolution structural MRI scans, the team applied advanced texture analytical algorithms to quantify microarchitectural variations across multiple brain regions implicated in visual perception and cognitive integration.
Statistical modeling revealed that alterations in brain texture significantly predicted the severity of visual perceptual dysfunctions across both cohorts. Notably, these texture anomalies localized to areas within the occipital cortex and associative visual pathways—regions essential for integrating sensory inputs into coherent perceptual experiences. This spatial specificity highlights a mechanistic link whereby microstructural brain changes may disrupt foundational sensory processing, cascading into complex cognitive and perceptual aberrations characteristic of psychosis.
Contrasting with traditional volumetric neuroimaging biomarkers that capture gross atrophy or enlargement, brain texture analysis provides a dimensional perspective of neural integrity by detecting subtle tissue heterogeneity potentially associated with cellular density, myelination patterns, and extracellular matrix alterations. These microscopic alterations may precede macroscopic lesions, marking brain texture as an exquisitely sensitive indicator of emerging neuropathology. The current findings suggest that early psychosis pathophysiology may involve microstructural disorganization affecting the fidelity of visual processing circuits before the establishment of widespread brain volume loss.
Furthermore, the research highlights the potential of texture-based biomarkers in stratifying risk and refining prognostic estimates in clinical high-risk populations. By integrating neuroimaging texture profiles with behavioral assessments, clinicians may better identify individuals on the cusp of transition to full-blown psychosis, enabling timely therapeutic interventions tailored to neurobiological vulnerabilities. This holds profound implications for personalized medicine approaches aiming to delay or prevent the onset of overt psychiatric disorders through early detection and targeted remediation.
Beyond diagnostic and prognostic utility, the study also sheds light on the underlying neurobiological mechanisms driving early psychosis. The brain texture patterns observed may reflect disrupted neural plasticity, aberrant synaptic pruning, or neuroinflammatory processes that compromise microstructural organization within sensory integration hubs. Such insights propel the field closer to unraveling the complex pathogenesis of psychotic disorders, moving beyond symptom-based classifications to biologically grounded frameworks that may guide novel treatment development.
The integration of multimodal neuroimaging with cutting-edge computational texture analysis represents a transformative advance in psychiatric neuroscience. Traditional imaging biomarkers have struggled with sensitivity and specificity, limiting their translational impact. In contrast, this texture-centric paradigm captures the nuanced alterations in brain microstructure that are fundamental to early disease processes. As machine learning and artificial intelligence algorithms further evolve, their synergy with texture analysis promises to unlock predictive models with unprecedented accuracy for mental health applications.
Critically, the study also emphasizes the importance of cross-disciplinary collaboration, merging expertise in neuroimaging physics, clinical psychiatry, computational modeling, and cognitive neuroscience. Such integrative approaches are essential for addressing the heterogeneity and complexity inherent in psychotic disorders. The methodological rigor and conceptual innovation embodied in this research set a new standard for future investigations aiming to decode the neural substrates of psychiatric illnesses.
Despite these promising findings, the researchers acknowledge limitations including sample size constraints and the need for longitudinal validation to confirm whether brain texture changes prognosticate disease progression or response to treatment. Expanding datasets with diverse populations and integrating additional modalities such as diffusion tensor imaging and functional MRI could deepen mechanistic understanding and boost clinical applicability. Nonetheless, this study represents a pivotal step forward, highlighting brain texture as a novel and potent marker for early psychosis detection.
In conclusion, the identification of brain texture alterations that predict subtle visual perceptual dysfunctions opens a new frontier in psychiatric diagnostics and neurobiological research. This approach provides a window into the microstructural brain changes that precede clinically apparent symptoms, offering hope for earlier intervention strategies that could transform outcomes for individuals vulnerable to psychotic disorders. As ongoing research builds on these insights, the vision of precision psychiatry grounded in detailed brain tissue characterization moves closer to reality, promising profound impacts on mental health care worldwide.
Subject of Research: Brain texture alterations and their predictive role in visual perceptual dysfunctions associated with recent onset psychosis and clinical high-risk states.
Article Title: Brain texture alterations predict subtle visual perceptual dysfunctions in recent onset psychosis and clinical high-risk state.
Article References:
Lencer, R., Sprenger, A., Meyhöfer, I. et al. Brain texture alterations predict subtle visual perceptual dysfunctions in recent onset psychosis and clinical high-risk state. Transl Psychiatry (2026). https://doi.org/10.1038/s41398-026-03840-x
Image Credits: AI Generated