In a groundbreaking study that promises to reshape neonatal care protocols, researchers have delved into the tangible effects of the American Academy of Pediatrics’ (AAP) 2022 revised clinical practice guidelines for managing neonatal hyperbilirubinemia. This highly specialized area of newborn care, marked by the accumulation of bilirubin leading to jaundice, has long demanded precise intervention to prevent dangerous complications such as kernicterus. The recent revisions aimed to refine existing strategies, but until now, the real-world impact of these updated guidelines on healthcare outcomes remained elusive. This pioneering investigation provides critical insights into how these guidelines influence post-discharge clinical visits and Neonatal Intensive Care Unit (NICU) readmissions related to hyperbilirubinemia, offering much-needed data on both effectiveness and healthcare system burden.
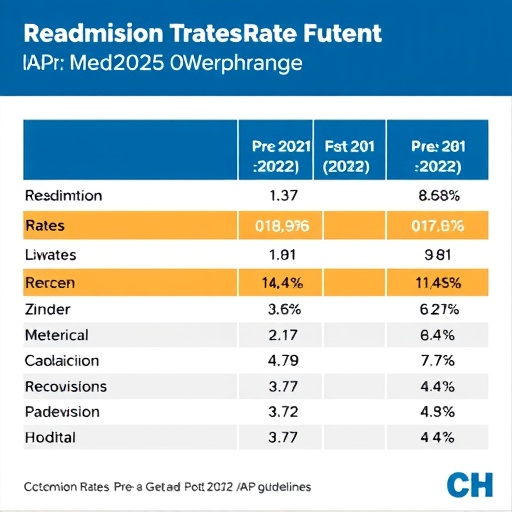
The study, conducted at a single center with a robust neonatal care unit, meticulously compared neonatal readmission rates and clinic follow-ups before and after implementation of the 2022 guidelines. Neonatal hyperbilirubinemia management involves intricate decision-making that balances treatment immediacy, discharge timing, and outpatient surveillance. Variations in criteria for identifying at-risk newborns directly impact healthcare resource utilization and patient safety. By aligning clinical practice with updated AAP protocols, clinicians aim to optimize this balance, reducing unnecessary readmissions while ensuring early detection of critical bilirubin elevations.
Fundamentally, the revised 2022 guidelines introduced more nuanced risk stratification tools and emphasized individualized care plans over broad, one-size-fits-all algorithms. These adjustments reflect a growing recognition of genetic, demographic, and clinical heterogeneity among neonates. The study’s authors dissected how risk-based recommendations altered thresholds for initiating phototherapy—a primary treatment modality for hyperbilirubinemia characterized by blue light exposure that converts bilirubin into water-soluble isomers for safe excretion. The meticulous analysis of patient cohorts, both prior to and following incorporation of the new guidelines, revealed subtle but significant shifts in clinical decision patterns.
One of the most notable findings relates to the timing and frequency of post-discharge follow-up visits. Prior to the 2022 revisions, standardized schedules often led to premature discharges or delayed recognition of worsening jaundice, resulting in reactive and sometimes preventable NICU readmissions. The revised guidelines aimed to minimize these pitfalls through evidence-based surveillance plans, promoting proactive identification of infants requiring immediate intervention. The study found that alignment with new protocols corresponded to a statistically significant decrease in emergency post-discharge clinic visits, suggesting more effective outpatient monitoring and parental education measures.
Parallel to changes in follow-up regimen, the research evaluated whether alterations in phototherapy initiation thresholds influenced readmission rates. Hyperbilirubinemia severity can escalate rapidly, and misjudgment of treatment necessity may either expose neonates to bilirubin toxicity or lead to excess hospital utilization. The study discerned a modest but meaningful reduction in NICU readmissions related to hyperbilirubinemia post-guideline implementation. This outcome supports the hypothesis that precise, nuanced risk assessment curbs unnecessary escalation of care, enabling safer outpatient management where appropriate.
However, the impact extended beyond mere numbers. The edited clinical guidelines fostered multidisciplinary collaboration, involving neonatologists, pediatricians, nurses, and family members, to create comprehensive care pathways. Such coordination ensures timely bilirubin measurement, feeding support to reduce enterohepatic circulation of bilirubin, and parental education on jaundice risk signs. The study emphasized this ecosystem of care improvements, highlighting their role in sustaining positive clinical outcomes and potentially reducing anxiety and stress associated with neonatal readmissions.
The researchers also noted important considerations regarding healthcare equity. By tailoring guidelines to better identify high-risk populations, including those from diverse ethnic backgrounds or with specific genotypes influencing bilirubin metabolism, the 2022 revisions helped address disparities in neonatal jaundice management. The study’s demographic analysis suggested more consistent care delivery across different socio-economic groups, indicating a vital step toward equitable neonatal healthcare provision.
Technological advancements intertwined with guideline changes further accentuate this evolution. Transcutaneous bilirubinometers, which offer rapid, non-invasive bilirubin measurements, were employed more systematically under the new protocols, enhancing early detection and reducing invasive blood sampling. The study linked this technological integration with improved adherence to recommended monitoring intervals, underscoring how technology can support guideline-driven improvements in patient care.
Despite the encouraging findings, the authors acknowledged limitations inherent in single-center, observational research. Local practice patterns, patient populations, and resource availability pose constraints on generalizability. Still, the rigorous methodology, comprehensive dataset, and clearly defined outcome measures lend credibility and urgency to the findings. These data serve as a critical foundation for multicenter, prospective trials that could further validate benefits and refine recommendations.
Moreover, the research illuminates potential future directions for neonatal hyperbilirubinemia management. Integration of machine learning algorithms analyzing vast clinical datasets could predict risk trajectories more precisely, customizing discharge and follow-up plans. Similarly, digital health tools could empower parents through real-time symptom tracking and direct communication channels with healthcare providers, enhancing home monitoring post-discharge.
This study resonates beyond the narrow confines of neonatal jaundice management, touching on broader themes in contemporary medicine: the importance of evidence-based guideline evolution, real-world validation, and iterative refinement of clinical practice to optimize outcomes and resource utilization. It exemplifies how seemingly incremental guideline updates can translate into meaningful reductions in avoidable hospitalizations and improvements in patient and family experiences.
In sum, the study by Otome, Adelowo, Farlett, and colleagues clarifies that the 2022 updated AAP hyperbilirubinemia guidelines have significantly influenced neonatal care at the clinical frontline. Their research underscores a decline in both hyperbilirubinemia-related NICU readmissions and post-discharge visits due to enhanced risk stratification and monitoring strategies. This success story highlights that diligent implementation and continuous evaluation of clinical guidelines remain crucial pillars in advancing neonatal health worldwide.
As neonatal mortality and morbidity remain key global health metrics, this investigation reaffirms that attention to conditions as common yet complex as jaundice can yield substantial public health dividends. Through systemic upgrades in detection, individualized treatment thresholds, and integrated follow-up protocols, the neonatal community can mitigate risks of long-term neurodevelopmental sequelae associated with bilirubin toxicity. The authors’ contribution thus extends an optimistic message: science-driven refinements in pediatric guidelines can dramatically improve early postnatal care trajectories.
Healthcare professionals and policy makers should view these findings as a call to action. Robust guideline dissemination, coupled with education for frontline workers and families, remains paramount. Meanwhile, investment in diagnostic technologies and care coordination frameworks is essential to sustain the positive trends observed. In the dynamic landscape of neonatal care, this study sets a new standard for evaluating guideline impact and shaping future innovations.
Ultimately, this research stands as a beacon encouraging the healthcare community to continue upgrading neonatal protocols in step with emerging evidence. The delicate balance of early discharge pressures and vigilant monitoring requires meticulous calibration that these 2022 AAP guidelines begin to achieve. Through sustained commitment to implementation fidelity and outcome surveillance, the promise of safer newborns and more efficient healthcare delivery draws nearer to realization. The study’s insights undoubtedly chart a promising pathway toward enhanced, patient-centered, and data-informed neonatal jaundice management worldwide.
Subject of Research: Impact of revised 2022 AAP clinical practice guidelines on post-discharge clinic visits and NICU readmissions related to neonatal hyperbilirubinemia.
Article Title: Readmission rates before and after the implementation of 2022 revised AAP clinical practice guidelines for the management of neonatal hyperbilirubinemia – a single center study.
Article References:
Otome, U., Adelowo, B., Farlett, R. et al. Readmission rates before and after the implementation of 2022 revised AAP clinical practice guidelines for the management of neonatal hyperbilirubinemia – a single center study. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02451-6
Image Credits: AI Generated
DOI: 08 December 2025