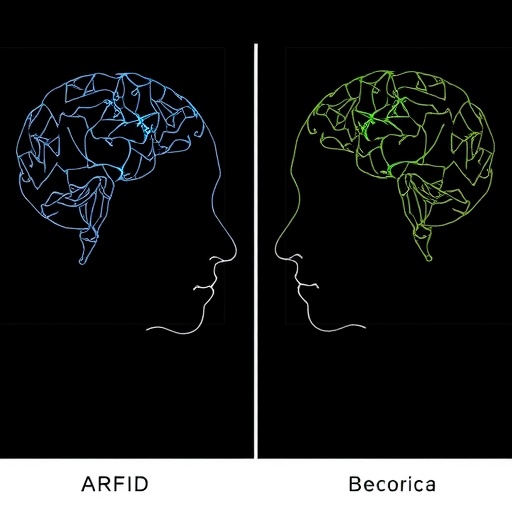
In a groundbreaking study published in the Journal of Eating Disorders, researchers have unveiled significant insights into the cognitive processes underlying two prominent eating disorders: Avoidant/Restrictive Food Intake Disorder (ARFID) and Anorexia Nervosa. This research, led by a team of esteemed experts including H. Wilkinson, A. Carbonnier, and H. Wilkinson-Herbots, delves into the complex world of eating disorder cognitions, aiming to discern the nuanced differences and similarities between these conditions. The findings not only illuminate the psychological landscapes of affected individuals but also have far-reaching implications for treatment strategies and therapeutic interventions.
Eating disorders, characterized by aberrant eating behaviors and profound psychological distress, represent a significant public health concern. Among them, Anorexia Nervosa has often been spotlighted due to its high mortality rate and severe physical consequences. However, ARFID has emerged as a distinct and prevalent disorder that warrants equal attention. Unlike Anorexia, which frequently revolves around body image distortions and a fear of weight gain, ARFID is primarily characterized by an extreme avoidance of certain foods, resulting in malnutrition and various health complications. This study’s comparative approach provides a crucial perspective on their distinct cognitive frameworks.
One of the pivotal findings of this research is the identification of distinct cognitive patterns associated with each disorder. Individuals with ARFID exhibit heightened sensitivity to food texture, flavor, and appearance, often resulting in an irrational aversion to certain food groups. This is not merely a phase of picky eating; rather, it profoundly impacts their daily lives and nutritional intake. In contrast, those suffering from Anorexia display a more pervasive focus on weight, shape, and self-worth, which intertwines deeply with social comparisons and self-esteem issues. Such cognitive dissimilarities underscore the necessity for tailored treatment modalities that address the individual needs of those struggling with these disorders.
The research also sheds light on the comorbidities commonly associated with these eating disorders. The team found that patients with ARFID frequently experience anxiety disorders, mood disturbances, and even sensory processing issues, complicating their relationship with food further. Conversely, those with Anorexia often grapple with mood disorders and obsessive-compulsive traits. Understanding these comorbidities is instrumental for clinicians as they develop comprehensive treatment plans that address the multifaceted nature of eating disorders.
Furthermore, the study raises important questions about the diagnostic criteria currently in use. The existing framework may not adequately capture the full spectrum of symptoms experienced by individuals with ARFID, leading to missed diagnoses and inadequate treatment. By comparing ARFID and Anorexia, the researchers advocate for a reevaluation of the diagnostic thresholds and criteria, emphasizing the importance of recognizing the unique challenges each disorder presents. A more nuanced diagnostic approach would ensure that patients receive the appropriate care and interventions they desperately need.
The implications of this research extend into the realm of therapeutic interventions as well. Understanding the cognitive mechanisms at play in ARFID and Anorexia can inform the development of specialized therapies. Cognitive-behavioral therapy (CBT), for example, could be adapted to target the specific cognitions associated with each disorder. In the case of ARFID, therapy could focus on gradually increasing food variety, addressing sensory sensitivities, and reducing anxiety surrounding mealtimes. For Anorexia, CBT might concentrate on challenging distorted beliefs about body image and weight, fostering healthier self-acceptance.
In addition to therapy, this research highlights the significance of support systems in the recovery process. The findings emphasize that individuals with ARFID and Anorexia do not exist in isolation; their experiences are deeply intertwined with family dynamics, peer relationships, and societal pressures. Family-based interventions, which actively involve loved ones in the recovery journey, could prove to be essential in fostering a supportive environment where individuals feel safe to explore their eating behaviors and underlying anxieties.
Moreover, the study underscores the need for educational initiatives aimed at parents, educators, and healthcare providers. Raising awareness about the cognitive aspects of ARFID and Anorexia can lead to earlier detection and intervention. The misconceptions that often surround eating disorders contribute to stigma and misunderstanding, preventing individuals from seeking help. By educating various stakeholders, society can create a more compassionate and informed landscape for those struggling with these complex conditions.
Another intriguing aspect of the research is its focus on the role of culture and societal influences in shaping eating disorders. Anorexia Nervosa, in particular, has been subject to cultural scrutiny, with societal beauty standards often exacerbating the disorder’s prevalence among young women. ARFID, however, may be more influenced by individual sensory experiences rather than social constructs. This divergence accentuates the need for cultural sensitivity in treatment approaches, ensuring they are not only evidence-based but also attuned to the specific cultural contexts of individuals.
As the research progresses, it is critical to continue exploring the biological underpinnings that may contribute to these disorders. Genetic factors, neurobiological processes, and hormonal influences on appetite and stress response can provide additional layers of understanding. The interplay between biology and psychology is intricate, and further investigations could unravel how these elements converge to affect eating behaviors, providing clearer pathways toward intervention.
The implications of these findings extend beyond individual treatment; they call for a systemic change in how eating disorders are conceptualized and treated. Advocacy for research funding, policy changes, and increased support for sufferers is paramount. As the stigma surrounding eating disorders diminishes, we may witness a shift in the societal perception of mental health issues, fostering an environment where individuals can seek help without fear of judgment.
In conclusion, this comprehensive study illuminates the complexities of eating disorder cognitions, offering a vital contribution to the field of mental health. The comparative analysis of ARFID and Anorexia Nervosa enriches our understanding of these conditions, paving the way for innovative treatment approaches and public discourse. By addressing the unique cognitions, comorbidities, and cultural contexts of both disorders, we are better equipped to support individuals on their path to recovery. The journey toward understanding and healing is ongoing, but through continued research and advocacy, we can foster a more inclusive and supportive environment for all those affected by eating disorders.
Subject of Research: Eating disorder cognitions in ARFID and Anorexia Nervosa
Article Title: Eating disorder cognitions: a comparison between Avoidant/Restrictive Food Intake Disorder (ARFID) and Anorexia Nervosa
Article References:
Wilkinson, H., Carbonnier, A., Wilkinson-Herbots, H. et al. Eating disorder cognitions: a comparison between Avoidant/Restrictive Food Intake Disorder (ARFID) and Anorexia Nervosa.
J Eat Disord 13, 262 (2025). https://doi.org/10.1186/s40337-025-01341-8
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s40337-025-01341-8
Keywords: Eating disorders, ARFID, Anorexia Nervosa, cognitive processes, treatment strategies, psychological distress, comorbidity, diagnostics, therapy, cultural influences.