In a groundbreaking study poised to reshape our understanding of traumatic brain injury (TBI), researchers have unveiled the pivotal role of the enzyme pyruvate kinase M2 (PKM2) within astrocytes and its profound influence on neuronal survival post-injury. This pioneering work elucidates cellular mechanisms that could forge new neuroprotective strategies, potentially transforming therapeutic approaches for millions worldwide who suffer from the devastating consequences of TBI.
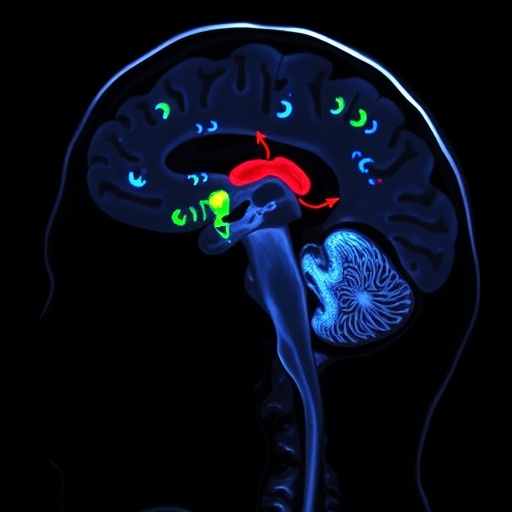
Traumatic brain injury remains one of the most challenging neurological disorders, marked by immediate neuronal loss and long-term cognitive and motor deficits. Despite advances in clinical management, effective treatments that target the molecular and cellular cascades following trauma remain elusive. The new study zeroes in on astrocytes—star-shaped glial cells traditionally regarded as mere support cells—highlighting their active participation in the brain’s response to injury and their unexpected role as modulators of neuronal fate.
Astrocytes, the most abundant cell type in the central nervous system, maintain homeostasis, regulate neurotransmitter levels, and provide metabolic support to neurons. Yet, this research reveals an even more intricate function: the expression of PKM2, an enzyme involved in glycolysis, which appears to be crucial for the astrocytes’ response to TBI. PKM2’s role extends beyond metabolism, influencing gene expression and cellular signaling pathways that dictate cell survival or death.
The authors employed a sophisticated conditional gene deletion technique targeting PKM2 specifically in astrocytes within a mouse model of TBI. This approach enabled an unprecedented examination of astrocytic PKM2’s direct consequences on neuronal death following mechanical brain trauma. The results were illuminating: deleting PKM2 in astrocytes exacerbated neuronal loss and worsened neurological outcomes, challenging previous assumptions about astrocytic metabolism in brain injury contexts.
Further exploration revealed that astrocytic PKM2 modulates the inflammatory milieu following TBI. The absence of PKM2 led to an exaggerated inflammatory response characterized by elevated pro-inflammatory cytokines and reactive gliosis, contributing to neuronal apoptosis. These findings suggest that PKM2 acts as a molecular switch, tempering inflammation and promoting neuroprotection through metabolic and non-metabolic pathways.
Moreover, the study detailed alterations in astrocyte-neuron metabolic coupling triggered by PKM2 deletion. Normally, astrocytes support neurons via lactate shuttling, sustaining neuronal energy demands especially under stress conditions like TBI. The loss of PKM2 impaired this metabolic cooperation, depriving neurons of critical energetic substrates and thereby accelerating cell death.
The data also implicated PKM2 in gene regulatory networks within astrocytes. The enzyme participates in epigenetic modulation and transcriptional regulation impacting survival-related genes. The study demonstrated that without this regulatory function in astrocytes, the expression of neuroprotective factors diminished, tipping the balance towards neurodegeneration.
Intriguingly, this research identified downstream signaling cascades influenced by PKM2, including pathways associated with oxidative stress and apoptosis. PKM2 appeared to mitigate oxidative damage by regulating antioxidant defenses, underscoring its role as a guardian molecule against secondary injury mechanisms that often propagate neuronal death days after the initial trauma.
Functional assessments confirmed that animals lacking astrocytic PKM2 exhibited worsened motor coordination and cognitive deficits, linking molecular changes to meaningful behavioral impairments. This translational aspect underscores the clinical relevance of the findings and opens avenues for targeting astrocytic metabolism to improve outcomes in TBI patients.
The implications of this work extend beyond TBI, shedding light on astrocyte biology in neurodegenerative diseases where metabolic dysfunction and inflammation drive pathology. Modulating PKM2 activity or expression in astrocytes may, therefore, represent a novel therapeutic axis transcending a single disease paradigm.
While the study presents compelling evidence, it also raises captivating questions about the precise mechanisms by which PKM2 orchestrates astrocyte functions and how this knowledge can be harnessed in clinical settings. Future research is needed to identify pharmaceutical agents capable of enhancing astrocytic PKM2 activity or mimicking its protective effects without compromising essential glycolytic functions.
This landmark study underscores the critical nature of metabolic enzymes as multifunctional regulators within brain cells and highlights the delicate interplay between metabolism, inflammation, and neuronal survival. As the neuroscience community continues to unravel astrocyte complexities, PKM2 emerges as a beacon of hope for developing interventions that could mitigate the often irreversible damage wrought by traumatic brain injuries.
In conclusion, the elucidation of astrocytic PKM2’s role represents a major leap forward in neurobiology, revealing novel pathways for protecting neurons from trauma-induced death. This paradigm shift invites renewed focus on glial biology in neurologic disease and exemplifies how targeting cellular metabolism can transcend traditional treatment boundaries, offering new horizons for both research and therapy.
As the incidence of TBI rises globally, particularly among younger populations and the elderly, the urgency for innovative treatments becomes ever more pronounced. The insights gleaned from this study not only deepen our scientific understanding but also provide a tangible foundation upon which future neuroprotective strategies can be constructed, promising hope to those affected by brain trauma worldwide.
The remarkable convergence of metabolism, gene regulation, and inflammation in a single enzyme within astrocytes opens exciting therapeutic possibilities. By modulating PKM2-mediated pathways, it may be feasible to develop drugs that fine-tune astrocyte functions, curbing detrimental inflammation and bolstering neuronal resilience in the injured brain.
Ultimately, this study exemplifies the power of cutting-edge genetic tools to dissect cellular interactions in complex diseases and reinforces the critical importance of astrocytes in maintaining neuronal integrity. As we move forward, embracing the neuron-glia partnership in brain injury will be paramount for transforming care and improving lives after TBI.
Subject of Research: Effects of astrocytic PKM2 gene deletion on neuronal death following traumatic brain injury
Article Title: Effects of astrocytic PKM2 gene deletion on neuronal death following traumatic brain injury
Article References: Kang, B.S., Park, M.K., Yang, H.W. et al. Effects of astrocytic PKM2 gene deletion on neuronal death following traumatic brain injury. Cell Death Discov. 11, 525 (2025). https://doi.org/10.1038/s41420-025-02829-7
Image Credits: AI Generated
DOI: 10 November 2025