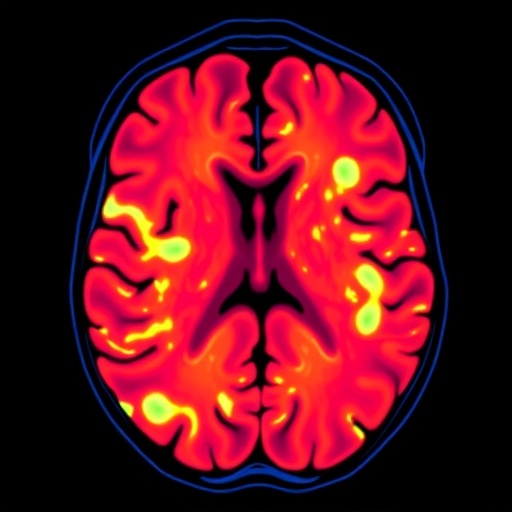
In a groundbreaking advancement in breast cancer diagnostics, researchers have unveiled a novel predictive model that combines traditional radiomics with state-of-the-art deep learning techniques applied to dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI). This innovative approach aims to non-invasively predict pathological complete response (pCR) in breast cancer patients undergoing neoadjuvant therapy (NAT), a critical factor in tailoring surgical and therapeutic strategies to enhance patient outcomes.
Breast cancer treatment increasingly depends on precision medicine approaches, where understanding tumor response to preoperative therapies profoundly impacts clinical decision-making. Neoadjuvant therapy, administered before surgery to shrink tumors, poses a significant challenge owing to the difficulty in predicting which patients will achieve complete eradication of cancer cells, defined as pCR. Existing assessment tools often lack sufficient accuracy or require invasive procedures, calling for sophisticated imaging biomarkers that can reliably forecast treatment success.
Utilizing a large retrospective cohort of 234 patients from two different medical institutions, the study meticulously integrated diverse data sources to construct and validate predictive models. The primary dataset, consisting of 204 cases, facilitated model training, while an independent external dataset of 30 patients served as a rigorous test bed to evaluate generalizability. This dual-cohort design strengthens the findings and minimizes bias often encountered in single-center studies.
Traditional radiomics involves extracting quantitative features from medical images that characterize tumor heterogeneity, shape, and texture. However, these features alone can capture only a fraction of the full complexity inherent in tumor biology. To transcend this limitation, the researchers incorporated three-dimensional deep learning features derived from both the entire DCE-MRI volume and focused tumor regions. This fusion enabled the model to harness subtle imaging cues and spatial relationships invisible to conventional methods.
Critically, the investigation focused on two distinct temporal phases of the DCE-MRI scans—the early enhancement phase and the peak enhancement phase. These intervals reflect different physiological and vascular properties of the tumor microenvironment, providing complementary insights into tumor perfusion and permeability. By merging features from these phases, the team hypothesized that predictive accuracy could be significantly bolstered.
Feature selection methodology was rigorous and multi-tiered. The researchers first applied independent sample t-tests to reduce feature redundancy and eliminate statistically insignificant variables. Subsequently, least absolute shrinkage and selection operator (LASSO) regression refined the feature set further by penalizing less informative predictors. The final model utilized the top ten most discriminative features, balancing complexity and overfitting risks effectively.
Logistic regression models were constructed to combine the chosen features and compute the probability of a patient achieving pCR. Model performance was quantified using receiver operating characteristic (ROC) curves and the corresponding area under the curve (AUC) metric, which captures overall discriminative ability. The DeLong test provided a statistical framework to compare AUC values across different models, confirming the superiority of integrated feature approaches.
The results revealed that models based solely on traditional radiomics features from combined early and peak DCE-MRI phases already demonstrated promising predictive power. However, the performance was markedly enhanced by augmenting these with deep learning features, culminating in the RD_EP model. This integrated model achieved impressive AUCs of 0.892 on the training dataset and 0.825 on the external validation cohort, indicating robust generalization and clinical utility potential.
Further elucidation of the model’s decision process was provided by SHapley Additive exPlanations (SHAP) analysis. This state-of-the-art interpretability tool highlighted that two specific radiomics texture features were predominant contributors to prediction accuracy. Understanding which features drive model outputs is pivotal for clinical acceptance, enabling oncologists to trust and integrate AI-driven tools into routine practice.
The implications of this study are profound. By accurately identifying patients who will respond favorably to NAT, clinicians can avoid overtreatment in responders and tailor intensified regimens or alternative therapies for non-responders. This personalized approach could translate into reduced surgical morbidity, optimized use of medical resources, and improved survival rates.
Moreover, the incorporation of multi-phase imaging and diverse feature extraction methodologies exemplifies the future trajectory of oncologic imaging. It underscores the significance of temporal dynamics in tumor physiology, encouraging further research into temporal radiomics and deep learning applications across cancer types and imaging modalities.
Despite its strengths, the study has areas requiring future exploration. Expanding sample sizes, including more diverse patient populations, and integrating additional molecular or genomic data could further enhance model accuracy. Prospective validation in clinical trial settings would also solidify the model’s applicability and impact on treatment decision algorithms.
This integration of advanced computational techniques with sophisticated imaging datasets represents a paradigm shift in breast cancer management, paving the way for more intelligent, less invasive, and highly personalized therapeutic strategies. As imaging technology and artificial intelligence rapidly evolve, such interdisciplinary approaches will likely redefine the biomarker landscape in oncology.
In summary, the research led by Zhang, Cai, Cui, and colleagues exemplifies cutting-edge efforts to harness the synergy between radiomics and deep learning applied to DCE-MRI at multiple temporal phases. Their work offers a promising avenue toward real-time, non-invasive prediction of neoadjuvant therapy outcomes in breast cancer—a critical step towards genuinely personalized medicine.
The future of breast cancer care lies in precision diagnostics harnessed through multidisciplinary innovation, and this study constitutes a significant leap forward. It sets a compelling precedent for the continued fusion of imaging science, artificial intelligence, and clinical oncology for the benefit of patients worldwide.
As these technologies become increasingly accessible, patients will benefit from more tailored treatment plans, ultimately leading to better prognoses and quality of life. This model could soon become a staple in breast cancer centers globally, informing decisions and improving outcomes with unprecedented confidence.
Such research not only advances our understanding but also showcases the transformative potential of deep learning-driven radiomics as a cornerstone in the era of personalized cancer therapy.
Subject of Research: Predicting pathological complete response (pCR) to neoadjuvant therapy in breast cancer patients by integrating radiomics and deep learning features from early and peak phases of dynamic contrast-enhanced MRI.
Article Title: Predicting breast cancer response to neoadjuvant therapy by integrating radiomic and deep-learning features from early-and-peak phases of DCE-MRI.
Article References:
Zhang, Y., Cai, J., Cui, C. et al. Predicting breast cancer response to neoadjuvant therapy by integrating radiomic and deep-learning features from early-and-peak phases of DCE-MRI. BMC Cancer 25, 1747 (2025). https://doi.org/10.1186/s12885-025-15095-8
Image Credits: Scienmag.com
DOI: 11 November 2025