In a groundbreaking development that promises to reshape therapeutic strategies for Alzheimer’s disease, scientists have unveiled a novel method using individualized functional connectome biomarkers to predict patient responses following repetitive transcranial magnetic stimulation (rTMS) treatment. This advancement offers a pivotal stride towards precision medicine in neurodegenerative disorders, where tailored interventions could revolutionize symptom management and disease progression.
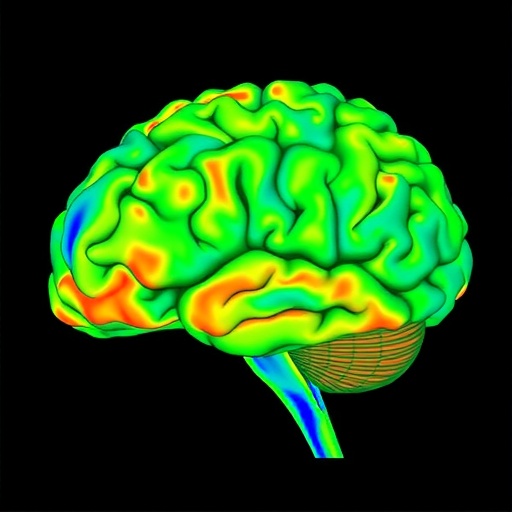
The study, led by a multidisciplinary team of neuroscientists and clinicians, delves deep into the intricate architecture of the brain’s functional connectome — a comprehensive map describing neural connections and their dynamic interactions. Through sophisticated neuroimaging techniques combined with machine learning algorithms, the research presents a highly individualized approach to discerning biomarkers that forecast clinical outcomes post-rTMS intervention in Alzheimer’s patients.
Repetitive transcranial magnetic stimulation, a non-invasive brain stimulation technique, has garnered attention for its potential to modulate neural circuits disrupted in Alzheimer’s. However, variability in treatment efficacy has posed significant challenges, impeding its broader clinical adoption. The variability largely stems from the heterogeneity in brain connectivity patterns among patients. By focusing on individualized connectomes, the researchers aimed to circumvent this obstacle, offering a predictive framework that tailors therapeutic courses to each patient’s unique neural landscape.
At the core of the study is the integration of functional magnetic resonance imaging (fMRI) data to map brain activity and connectivity across multiple regions implicated in cognitive decline. These maps provide a rich dataset capturing the temporal dynamics of neural interactions, which are then analyzed to extract biomarkers reflecting the brain’s response to rTMS. The biomarkers not only indicate immediate functional changes but also correlate with longitudinal clinical symptom improvements or declines.
The methodological innovation lies in applying advanced computational techniques to this vast neuroimaging dataset. Utilizing machine learning, the team developed predictive models that assess how specific patterns within a patient’s connectome relate to their clinical trajectory following rTMS treatment. This modeling takes into account complex, nonlinear relationships and potential confounds, ensuring robust, generalizable predictions beyond traditional analytical methods.
Critically, the biomarkers identified are individualized, meaning each patient’s unique brain connectivity blueprint informs the prediction of how their symptoms might evolve after stimulation therapy. This contrasts starkly with previous approaches that relied on group-based markers, often overlooking subtle yet crucial inter-individual neural differences. The personalized approach holds promise not only for optimizing treatment plans but also for uncovering new therapeutic targets within the brain’s network architecture.
The clinical implications of this research are profound. Alzheimer’s disease, characterized by progressive cognitive and functional decline, currently lacks effective disease-modifying treatments. Symptomatic relief through rTMS has been sporadic and unpredictable. With connectome-based biomarkers, clinicians may soon predict who stands to benefit most from rTMS, adjust protocols in real-time, and monitor treatment efficacy with unprecedented precision.
Moreover, the study paves the way for deploying such biomarkers in routine clinical practice, potentially transforming how neurodegenerative diseases are managed. Early identification of responders and non-responders to stimulation therapies could reduce trial-and-error prescribing, minimize side effects, and lead to better allocation of healthcare resources.
Importantly, the research emphasizes the dynamic nature of the brain’s connectome. Alzheimer’s pathology affects neural networks progressively, and the functional connectome evolves over time. By capturing these temporal dynamics, the biomarkers can track disease progression and treatment response concurrently, offering a dual utility rarely achieved in neuropsychiatric research.
The work’s integration of high-dimensional data analysis with clinical neurology exemplifies the growing synergy between computational neuroscience and patient-centered care. It also highlights the value of interdisciplinary collaboration, bringing together neuroimaging specialists, data scientists, and clinicians to tackle one of medicine’s most daunting challenges.
While the results are promising, the authors caution that broader validation across diverse populations and longitudinal follow-up are imperative. Alzheimer’s disease manifests heterogeneously across ethnicities, genetic backgrounds, and environmental factors, necessitating model refinement to ensure equitable applicability.
Beyond Alzheimer’s, the conceptual framework of individualized functional connectome biomarkers holds potential across a spectrum of neuropsychiatric disorders where electrical or magnetic brain stimulation is employed. Conditions such as major depressive disorder, Parkinson’s disease, and epilepsy might similarly benefit from personalized predictive tools guiding neuromodulation therapies.
In sum, this pioneering research marks a decisive step toward unlocking the full potential of rTMS in Alzheimer’s care through the lens of the individualized brain. It opens a new chapter in precision neuromedicine, where detailed maps of neural connectivity direct tailored interventions, enhancing outcomes and bringing hope to millions affected by neurodegeneration.
The convergence of advanced brain mapping, predictive analytics, and therapeutic neuromodulation embodied in this study heralds a transformative era in neuroscience. As technology continues to evolve, so too will our capability to decipher and harness the brain’s complex network, ultimately translating into meaningful clinical breakthroughs.
Future directions will likely explore integrating genetic, molecular, and behavioral data alongside connectome biomarkers to create even richer predictive frameworks. Such multidimensional models promise a holistic understanding of Alzheimer’s pathology and response to treatment, driving the evolution from symptomatic management to potentially curative strategies.
The ongoing challenge remains to translate these research insights into accessible clinical tools. This will require close collaboration between scientists, clinicians, regulatory bodies, and healthcare systems to ensure robust, validated biomarkers become part of standard care pathways.
In the meantime, this study serves as a beacon of innovation, demonstrating how harnessing the power of individualized brain connectivity can illuminate paths toward personalized therapies, improved patient outcomes, and ultimately, a future where Alzheimer’s disease is better understood and more effectively treated.
Subject of Research: Alzheimer’s disease, individualized functional connectome biomarkers, predictive modeling, repetitive transcranial magnetic stimulation (rTMS), neurodegenerative disorder therapy.
Article Title: Individualized functional connectome biomarkers predict clinical symptoms after rTMS treatment in Alzheimer’s disease.
Article References:
Yang, C., Wang, P., Zhu, Z. et al. Individualized functional connectome biomarkers predict clinical symptoms after rTMS treatment in Alzheimer’s disease. Transl Psychiatry (2025). https://doi.org/10.1038/s41398-025-03726-4
Image Credits: AI Generated