In a groundbreaking advancement in oncological diagnostics, researchers have unveiled a sophisticated deep learning fusion model that harnesses ultrasound imaging to predict early tumor response in breast cancer patients undergoing neoadjuvant chemotherapy (NAC). This pioneering study, conducted across two major medical centers, integrates cutting-edge artificial intelligence with radiomics to offer a promising new avenue for personalized cancer treatment planning.
The impetus behind this research stems from the critical need to identify how breast tumors respond to NAC at the earliest possible stage. Traditionally, clinicians rely on physical examinations and imaging after several chemotherapy cycles to assess tumor shrinkage or progression. However, these approaches often come too late to adapt treatment strategies effectively. By capitalizing on ultrasound images taken after just two cycles of chemotherapy, the researchers aim to revolutionize this timeline, enabling oncologists to predict responsiveness far earlier.
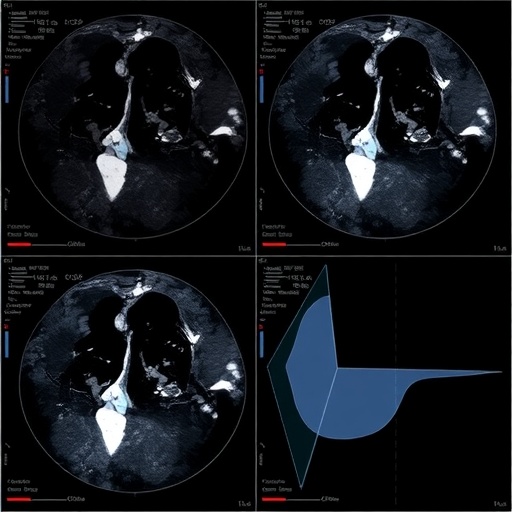
Central to this innovation is the application of ResNet, a deep learning architecture renowned for its ability to extract intricate features from complex image data. The team meticulously analyzed ultrasound images focusing on both the intratumoral region—the core of the tumor—and the peritumoral area, which encompasses the tissue surrounding the tumor. This dual-region approach acknowledges the tumor microenvironment’s role in cancer progression and therapeutic resistance, a factor often overlooked in conventional imaging analyses.
To elevate predictive accuracy, the researchers implemented stacking fusion technology. This technique synergistically combines models trained on different regions of interest (ROIs) within the ultrasound data—specifically, the intratumoral area and concentric peritumoral zones of 3 mm, 5 mm, and 10 mm radii. Such stacking fusion amalgamates distinct predictive signals, resulting in a robust model that outperforms single-region analyses individually.
The comprehensive dataset comprised 469 breast cancer patients treated with six to eight NAC cycles from May 2019 to September 2023. Partitioned into training, internal validation, and external validation cohorts, the model underwent rigorous testing to ascertain its generalizability across diverse clinical settings. The performance metric of choice, the area under the receiver operating characteristic curve (AUC), provided quantitative insights into prediction precision.
Remarkably, the fusion model, denoted DLRS3, demonstrated impressive AUC values across all datasets and ROI configurations. In the training set, AUCs ranged from 0.848 for the intratumoral region to an outstanding 0.919 for the 10 mm peritumoral ROI, indicating exceptional discrimination between responders and non-responders to NAC. These findings were echoed in the internal validation set, with the 5 mm ROI achieving an exceptionally high AUC of 0.965. The external validation, critical for confirming model portability, reaffirmed robust performance with AUCs reaching up to 0.938 for the 10 mm peritumoral region.
Beyond statistical metrics, the study employed clinical decision curve analysis (DCA) to evaluate the practical net benefit of deploying this model in patient care. The results signified that the fusion model could significantly enhance decision-making by guiding clinicians towards tailored therapeutic adjustments, potentially sparing patients from ineffective treatments and their associated toxicities.
Technologically, this research exemplifies the power of integrating advanced deep learning frameworks with medical imaging to decipher complex biological signals. The use of ultrasound, a non-invasive, widely accessible imaging modality, further underscores the clinical relevance and feasibility of this approach. Unlike more expensive or less available imaging techniques like MRI or PET, ultrasound can be repeatedly used with minimal risk, supporting dynamic monitoring during NAC.
Furthermore, the dual-center design lends robustness to the study, capturing variability across different patient populations, ultrasound equipment, and clinical protocols. This diversity fortifies the model’s translational potential, suggesting it could be adapted for widespread clinical integration, pending further prospective validation.
The insight into peritumoral tissue’s predictive value opens new research pathways to understand how tumor-stroma interactions influence chemotherapy efficacy. Such knowledge could inspire adjunct therapies aimed at modulating the tumor microenvironment to enhance treatment response.
The implications of this research extend beyond breast cancer. The methodologies showcased—deep learning, stacking fusion, dual-region radiomics—may be adapted to other malignancies where early treatment response prediction remains a challenge. This paradigm shift towards precision oncology embodies the future of cancer care.
In conclusion, this dual-center study represents a milestone in oncological diagnostics by delivering a novel deep learning fusion model that leverages early-cycle ultrasound imaging to accurately forecast breast cancer patients’ responses to neoadjuvant chemotherapy. By facilitating prompt, individualized treatment modifications, this technology holds promise to improve patient outcomes and catalyze a new era of intelligent cancer management.
Subject of Research: Predicting early tumor response in breast cancer patients receiving neoadjuvant chemotherapy using ultrasound-based deep learning radiomics models.
Article Title: Predicting breast cancer response to neoadjuvant chemotherapy with ultrasound-based deep learning radiomics models —— dual-center study
Article References:
Liu, J., Leng, X., Yuan, Z. et al. Predicting breast cancer response to neoadjuvant chemotherapy with ultrasound-based deep learning radiomics models —— dual-center study. BMC Cancer 25, 1737 (2025). https://doi.org/10.1186/s12885-025-15148-y
Image Credits: Scienmag.com
DOI: 10.1186/s12885-025-15148-y