In a groundbreaking study published in Nature Communications, researchers have unveiled new prognostic biological subtypes in Mantle cell lymphoma (MCL) by integrating functional genomics with detailed analyses of the tumor microenvironment. This innovative approach has the potential to transform how clinicians understand and manage this aggressive form of non-Hodgkin lymphoma, ultimately paving the way for more personalized treatment strategies.
Mantle cell lymphoma, a rare but aggressive B-cell malignancy, has long challenged oncologists due to its clinical heterogeneity and poor prognosis. Despite advances in treatment, outcomes vary widely among patients, largely because of the complex molecular and cellular interactions underpinning tumor behavior. The research team, led by Sharma, Ali, and Bouska, leveraged state-of-the-art functional genomics techniques alongside high-resolution profiling of the microenvironment to decode the biological intricacies driving MCL progression.
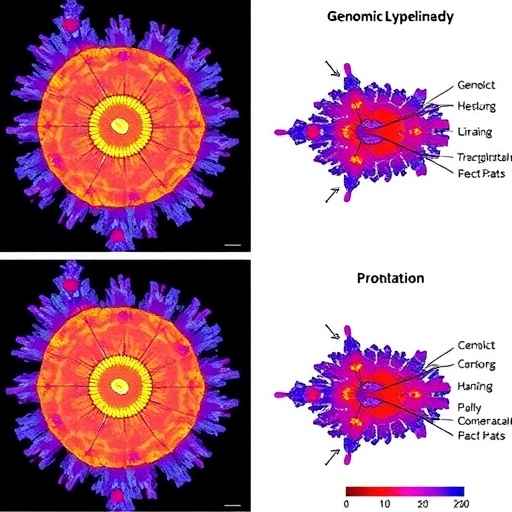
The study employed comprehensive genomic sequencing to uncover genetic alterations functionally impacting the tumor cells. This approach went beyond mere identification of mutations by systematically assessing their biological consequences on gene expression and cellular pathways. It revealed that MCL tumors could be stratified into distinct biological subtypes based on their unique genetic and transcriptomic landscapes. These subtypes were characterized by differential activation of oncogenic networks, including pathways involved in cell cycle regulation, DNA damage response, and immune evasion mechanisms.
Complementing the genomic analysis, the researchers meticulously characterized the tumor microenvironment—the complex milieu of immune cells, stromal elements, and signaling molecules surrounding malignant cells. Utilizing advanced single-cell RNA sequencing and multiplex immunohistochemistry, they delineated how distinct microenvironmental compositions correlated with the identified MCL subtypes. Notably, certain subtypes displayed an immunosuppressive milieu featuring regulatory T cells and myeloid-derived suppressor cells, while others exhibited a pro-inflammatory context enriched for cytotoxic T lymphocytes.
A pivotal discovery from this dual genomic and microenvironmental profiling was the identification of prognostic biological subtypes that significantly predicted clinical outcomes. Patients harboring tumors with an immune-evasive microenvironment and pronounced genetic disruptions in DNA repair genes tended to have poorer survival rates. Conversely, subtypes marked by heightened immune activation and intact genomic stability were associated with more favorable prognoses. This nuanced stratification holds immense promise for guiding precision therapies and risk-adapted treatment intensification.
The implications of these findings extend beyond prognostication. By mapping functional genomic alterations onto biological pathways, the study suggests actionable targets for emerging therapies. For example, subtypes showing deregulation of cell cycle proteins like cyclin D1 and CDK4 pinpoint vulnerabilities for selective CDK inhibitors. Similarly, the characterization of an immunosuppressive tumor microenvironment lays the foundation for combining immune checkpoint blockade with agents that modulate tumor-associated macrophages.
From a technical standpoint, the integration of multi-omics data sets poses significant analytical challenges that the team adeptly addressed through machine learning algorithms and network analysis. This enabled the extraction of biologically meaningful patterns from voluminous data, illustrating the critical role of computational biology in contemporary cancer research. By combining bulk and single-cell omics, the study captures both the macro-level genomic aberrations and the micro-level cellular heterogeneity defining MCL biology.
Such advances underscore the increasing relevance of systems biology approaches in oncology, where dissecting tumor heterogeneity remains a paramount obstacle. Traditional classifications based on morphology or limited molecular markers fall short in capturing the dynamic and adaptive nature of cancers like MCL. This integrative methodology transcends those limitations by providing a multi-dimensional view that links molecular alterations to their functional consequences within the spatial and immunological context of the tumor.
Clinically, these insights beckon a new era of biomarker-driven trials where patients can be stratified by their tumor’s biological subtype rather than broadly defined disease categories. Future clinical protocols could incorporate subtype-specific endpoints for evaluating novel targeted therapies or immunomodulatory treatments, enhancing precision medicine frameworks. Moreover, the ability to identify aggressive tumors at diagnosis may prompt earlier intervention with intensified regimens, potentially improving long-term survival.
The study further accentuates the importance of tumor-immune interactions in MCL pathogenesis. Immune evasion emerges as a central hallmark, with tumor cells sculpting their microenvironment to escape immune surveillance. This recognition aligns with growing evidence across various cancers, emphasizing that successful therapeutic strategies must concurrently target tumor-intrinsic genetic abnormalities and their immunological niches.
In sum, Sharma and colleagues deliver not only a comprehensive atlas of the functional genomics and microenvironmental features in Mantle cell lymphoma but also a clinically actionable framework to redefine its biological subtyping. These discoveries herald a shift toward more refined diagnostic categories and personalized therapeutic pipelines, potentially elevating patient care standards in this challenging lymphoma subtype.
As we stand on the cusp of integrating multi-omic insights into routine clinical practice, this study exemplifies how complex cancer biology can be unraveled through interdisciplinary collaboration. MCL patients, clinicians, and researchers alike may soon benefit from these novel stratifications that bring us closer to decoding the full spectrum of lymphoma heterogeneity and tailoring treatments with unprecedented specificity.
The road ahead involves validating these subtypes in larger cohorts and exploring their predictive power for response to existing and emerging therapies. Additionally, unraveling the mechanisms underpinning subtype-specific microenvironment remodeling could unlock new immunotherapeutic avenues. Ultimately, this work reaffirms that the future of lymphoma research lies in embracing complexity, leveraging technology, and fostering a dynamic interface between bench and bedside.
Subject of Research: Mantle cell lymphoma, Functional genomics, Tumor microenvironment, Prognostic subtypes
Article Title: Functional genomics and tumor microenvironment analysis reveal prognostic biological subtypes in Mantle cell lymphoma
Article References: Sharma, S., Ali, R., Bouska, A. et al. Functional genomics and tumor microenvironment analysis reveal prognostic biological subtypes in Mantle cell lymphoma. Nat Commun 16, 9762 (2025). https://doi.org/10.1038/s41467-025-64666-7
Image Credits: AI Generated