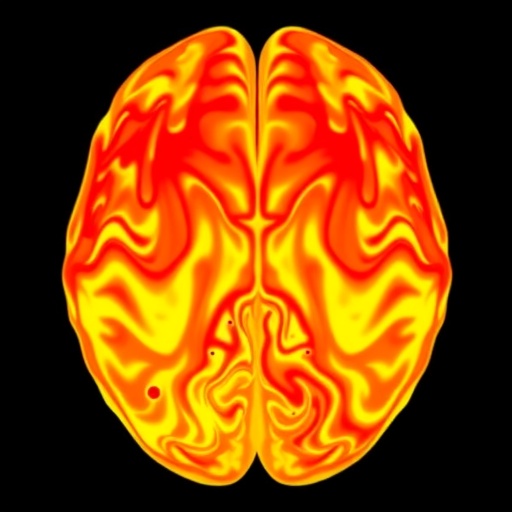
In a groundbreaking study set to transform our understanding of Parkinson’s disease, researchers have unveiled striking alterations in cerebrovascular haemodynamics through the use of 4D flow magnetic resonance imaging (MRI). This cutting-edge investigative technique has provided unprecedented insights into the dynamic blood flow patterns within the brains of Parkinson’s patients, opening new avenues for diagnosis and therapeutic strategies. Parkinson’s disease, long known primarily for its motor symptoms resulting from dopaminergic neuron loss, may now be understood through an expanded lens that includes vascular contributions to its pathophysiology.
The complexity of cerebral blood flow regulation has often been overlooked in neurodegenerative disease research. Traditional imaging modalities have lacked either the resolution or dynamic capabilities to adequately capture the nuanced disturbances occurring at the microvascular and macrovascular levels simultaneously. The utilization of 4D flow MRI represents a pivotal development. By acquiring volumetric, time-resolved velocity data, this technique characterizes multidirectional blood flow velocities throughout the cardiac cycle, enabling a comprehensive assessment of cerebrovascular biomechanics previously unattainable.
In Parkinson’s disease, motor impairment has predominantly been ascribed to the degeneration of substantia nigra neurons, yet mounting evidence suggests that cerebrovascular integrity plays an equally critical role. The research team, led by Deane, Myall, and Pilbrow, has demonstrated that patients exhibit significant deviations in haemodynamic parameters compared with healthy controls. These include altered flow velocity profiles, disturbed pulsatility indices, and impaired coupling between systemic cardiac output and cerebral perfusion. Such deviations could exacerbate neuronal vulnerability by compromising oxygen and nutrient delivery, thereby accelerating disease progression.
The findings underscore that Parkinson’s is not solely a neurocentric disorder but also involves vascular contributions that interact synergistically with neurodegeneration. Importantly, this study documents how specific intracranial arteries—the middle cerebral artery and the basilar artery, among others—show aberrant flow dynamics when measured in four spatial dimensions plus time. Disturbances in these critical conduits manifest as irregular shear stress patterns on endothelial surfaces, potentially triggering inflammatory cascades and blood-brain barrier dysfunction, phenomena rarely detectable by conventional imaging.
Technically, 4D flow MRI exploits phase-contrast imaging principles to encode velocity vectors within three orthogonal directions at each voxel throughout cardiac cycles. Unlike static angiography or Doppler ultrasound, this four-dimensional imaging provides the velocity vector field with high spatial and temporal resolution. This enables reconstruction of hemodynamic parameters such as wall shear stress and flow turbulence, which are crucial to vascular health but have remained largely uncharted in Parkinson’s patients until now.
The study also elucidates how these haemodynamic changes correlate with clinical symptoms severity and disease duration, suggesting a potential role for vascular biomarkers in monitoring disease progression. The coupling of neuronal loss with compromised cerebrovascular flow dynamics could serve as a valuable prognostic tool, identifying at-risk patients earlier than symptom presentation alone. This represents a significant leap in precision medicine approaches, fostering tailored interventions addressing both vascular and neurodegenerative components.
Moreover, these haemodynamic insights open exciting therapeutic vistas. Modulation of cerebral blood flow through pharmacological or lifestyle interventions might mitigate vascular insults, potentially slowing neurodegeneration. Drugs aimed at improving endothelial function or reducing vascular inflammation could become adjunct therapies. The revelation that cerebrovascular impairment is deeply embedded in Parkinson’s pathophysiology redefines therapeutic targets beyond classical dopaminergic replacement therapies that alleviate symptoms but do not alter disease trajectory.
The study’s implications extend beyond neuroscience into imaging technology innovation. The robustness and reproducibility of 4D flow MRI in capturing detailed cerebrovascular alterations encourage its integration into routine clinical diagnostics. Future longitudinal studies deploying this technology could track haemodynamic changes pre-symptomatically, allowing earlier intervention and possibly prevention. Additionally, the approach may validate the efficacy of novel treatments by providing objective vascular flow metrics as outcome measures.
Another critical dimension highlighted is the interplay between systemic cardiovascular health and cerebral haemodynamics in Parkinson’s disease. The research reveals that cardiac function anomalies such as reduced stroke volume or arrhythmias further distort cerebral perfusion profiles. This systemic perspective emphasizes managing cardiovascular comorbidities to preserve cerebral function, underlining the necessity of multidisciplinary care paradigms in Parkinson’s management.
Despite these advances, challenges remain in translating 4D flow MRI findings into clinical practice. The high cost, time-intensive acquisitions, and computational demands for data reconstruction and analysis currently limit widespread accessibility. There is also a pressing need to establish standardized protocols and normative databases to differentiate pathological haemodynamics reliably. Nevertheless, ongoing technological improvements and machine learning algorithms hold promise to overcome these barriers rapidly.
Critically, this study intensifies the call for a holistic framework in neurological disease research that incorporates vascular biology, fluid mechanics, and neurodegeneration. Viewing Parkinson’s disease through this integrated prism not only deepens mechanistic understanding but also revitalizes hope for comprehensive interventions that can alter the natural history of this debilitating disorder. As the population ages and Parkinson’s prevalence climbs, these innovations could pivot health outcomes substantially.
The pioneering work conducted by Deane, Myall, Pilbrow, and colleagues thus ushers in a new era of cerebrovascular exploration in Parkinson’s disease. With 4D flow MRI as a window into the living brain’s vascular dynamics, the scientific and medical communities stand poised to unravel the vascular underpinnings of neurodegeneration with unprecedented clarity. This breakthrough embodies the promise of cutting-edge imaging technology coupled with translational neuroscience to confront one of humanity’s most challenging neurological disorders.
As researchers further refine these vascular imaging techniques and unravel the complex cerebrovascular networks involved in Parkinson’s, each blood pulse and flow pattern decoded may hold critical clues for halting or reversing neuronal damage. Such insights nourish optimism that soon, Parkinson’s will no longer be viewed as an inexorable loss of motor function but as a multisystem disorder amenable to multifaceted, targeted therapies. The vascular-nerve axis is finally receiving the scientific attention it deserves, charting a hopeful path towards more effective treatments and improved quality of life for millions worldwide.
Subject of Research: Cerebrovascular haemodynamics alterations in Parkinson’s disease using 4D flow MRI.
Article Title: Altered cerebrovascular haemodynamics in Parkinson’s disease: Insights from 4D flow MRI.
Article References:
Deane, A.R., Myall, D.J., Pilbrow, A. et al. Altered cerebrovascular haemodynamics in Parkinson’s disease: Insights from 4D flow MRI. npj Parkinsons Dis. (2026). https://doi.org/10.1038/s41531-026-01276-0
Image Credits: AI Generated