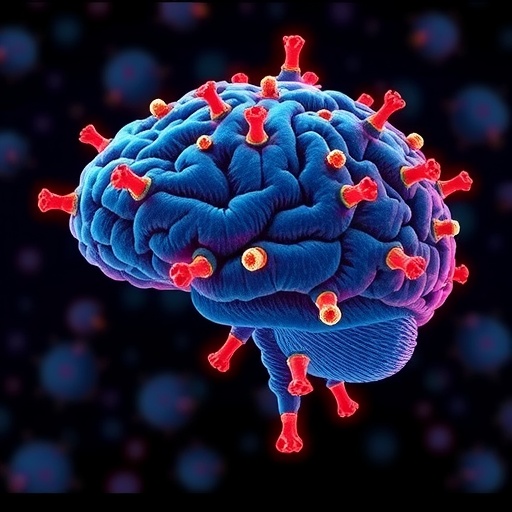
In a groundbreaking advancement in the fight against glioblastoma, a collaborative team of researchers from Mass General Brigham and the Dana-Farber Cancer Institute has demonstrated that a single injection of a genetically engineered oncolytic virus can profoundly reshape the tumor microenvironment, facilitating infiltration and persistence of immune cells deep within brain tumors. This significant discovery, detailed in a recent publication in the journal Cell, provides compelling evidence that such therapeutics can extend survival for patients afflicted with glioblastoma, a notoriously aggressive and lethal primary brain cancer with limited treatment options and bleak prognoses.
Glioblastomas have long been resistant to conventional immunotherapies that have revolutionized treatment paradigms in other cancers like melanoma. A central obstacle has been their status as “immune cold” tumors—an environment characterized by scant immune cell presence, particularly cytotoxic T lymphocytes, which are instrumental in targeting and destroying malignant cells. According to Dr. Kai Wucherpfennig, chair of the Department of Cancer Immunology and Virology at Dana-Farber and co-senior author of the study, the inability of immune effector cells to infiltrate these brain tumors has compromised therapeutic success. The new research overturns this limitation by demonstrating how oncolytic virotherapy can orchestrate a powerful immune infiltration, effectively turning these cold tumors into hotbeds of immune activity.
The therapeutic vector employed in the trial is a modified herpes simplex virus (HSV), painstakingly engineered to selectively replicate within glioblastoma cells while sparing healthy brain tissue. This tumor-tropic oncolytic virus exploits the vulnerabilities of cancer cells: upon infection, it hijacks the malignant cell’s machinery to replicate itself, resulting in the destruction of the infected cell. More than simply a cell-killing agent, the virus incites an immunogenic cascade, recruiting diverse components of the immune system into the tumor. The study’s Phase 1 clinical trial included 41 patients with recurrent glioblastoma, revealing that this oncolytic viral therapy significantly extended survival times compared to historical controls, particularly in individuals harboring pre-existing antibodies against the virus itself.
Underlying this clinical success is a meticulously conducted mechanistic inquiry. Utilizing sophisticated immunological and molecular analyses, the researchers mapped the immune landscape inside the tumors following treatment. They observed durable infiltration by activated cytotoxic T cells—immune warriors equipped to recognize and kill tumor cells. Intriguingly, these T cells exhibited sustained activity, maintaining cytotoxic effector functions long after the initial viral administration. A critical observation was the spatial correlation of these T cells with dying tumor cells, underscoring the immunotherapy’s direct cytolytic impact and linking immune invasion with patient survival. The data also showed that the therapy amplified resident T cell populations already present in the brain, enhancing the intrinsic immune surveillance of glioblastoma.
Dr. E. Antonio Chiocca, Executive Director at Mass General Brigham Cancer Institute and co-senior author, emphasized the transformative implications of the study. Glioblastoma has suffered from stagnation in treatment innovation for two decades, maintaining dismal survival rates despite aggressive interventions such as surgery, radiation, and chemotherapy. The capacity to safely and effectively inject a viral agent that recruits and activates immune cells inside the blood-brain barrier represents a paradigm shift, potentially opening new avenues for combinatorial therapies and personalized immuno-oncology regimens for these patients.
The engineered herpes simplex virus used—referred to as a genetically modified oncolytic HSV—has been rigorously designed to mitigate risks associated with viral infections of the central nervous system. Its tumor specificity arises from genetic modifications preventing replication in normal brain cells, conferring a favorable safety profile. Once inside the tumor microenvironment, the virus induces a multifaceted immune response extending beyond direct tumor lysis. It triggers the release of tumor antigens and danger signals, reshaping the immunosuppressive milieu characteristic of glioblastoma into an inflamed landscape conducive to immune cell recruitment and activation.
This study’s clinical and immunological insights underscore the dual mechanisms at play: oncolytic virotherapy not only executes direct cytotoxicity but also functions as an immune “primer,” stimulating antitumor immunity. The phase 1 trial results, supported by correlative immunophenotyping, collectively illustrate that a single dose can induce long-lasting immune activation capable of combating glioblastoma. This contrasts with previous therapeutic attempts that failed to overcome the tumor’s inherent immune evasion strategies, showcasing oncolytic viruses as potent mediators of immune modulation in the brain.
In examining patient heterogeneity, the study highlighted an intriguing association between pre-existing immunity against the viral vector and therapeutic efficacy. Patients possessing baseline antibodies against the herpes simplex virus exhibited improved survival outcomes, suggesting that the immune system’s prior sensitization may enhance or synergize with the viral therapeutic effect. Such observations underscore the need for deeper understanding of host-viral immune dynamics and may inform patient stratification and dosing schedules in future trials.
Moreover, the research team identified that the infiltrating T cells were not randomly distributed but localized in close proximity to apoptotic tumor cells, implying an on-target, antigen-specific immune response. These T cells demonstrated persistent activation markers and maintained their cytotoxic capabilities over extended periods post-treatment. Such long-term immune engagement is critical for durable tumor control and may underlie the survival benefit observed clinically.
This groundbreaking study was meticulously conducted with interdisciplinary expertise spanning immunology, virology, neuro-oncology, and translational medicine. It represents an exemplar of how innovative genetic engineering, coupled with clinical insight and advanced immunophenotyping technologies, can spearhead next-generation therapeutics for challenging malignancies like glioblastoma. The clinical implications reverberate beyond brain cancer, potentially catalyzing broader applications of oncolytic virotherapy in diverse tumor types traditionally refractory to immunotherapies.
Looking forward, the success of this trial paves the way for expanding oncolytic virus-based therapeutic protocols, including combination regimens with checkpoint inhibitors, CAR T cells, or standard therapies to augment efficacy. The promise of achieving sustained immune surveillance and tumor eradication in the hostile landscape of the central nervous system offers renewed hope for patients who face few otherwise effective treatments. Importantly, the safety profile combined with mechanistic clarity from this study establishes a robust platform for subsequent pivotal trials and regulatory advancement.
In summary, this pioneering research reveals that a single injection of an oncolytic herpes simplex virus can convert the immunologically cold environment of glioblastoma into one rich with activated, tumor-targeting cytotoxic T cells. This immune remodeling correlates with meaningful survival extension in patients, marking a momentous stride in neuro-oncology and cancer immunotherapy. With glioblastoma historically deemed near-impossible to treat, the novel strategy employed here reinvigorates optimism and underscores the power of harnessing viral vectors to enlist the body’s immune system against deadly brain tumors.
Subject of Research: People
Article Title: Persistent T cell activation and cytotoxicity against glioblastoma following single oncolytic virus treatment in a clinical trial
News Publication Date: 11-Feb-2026
Web References:
- Clinical trial information: https://clinicaltrials.gov/study/NCT03152318
- Published study DOI: https://doi.org/10.1016/j.cell.2025.12.055
References: Meylan M et al. “Persistent T cell activation and cytotoxicity against glioblastoma following single oncolytic virus treatment in a clinical trial” Cell 2026. DOI: 10.1016/j.cell.2025.12.055
Keywords: Glioblastomas, Brain cancer, Glioblastoma cells, Virology