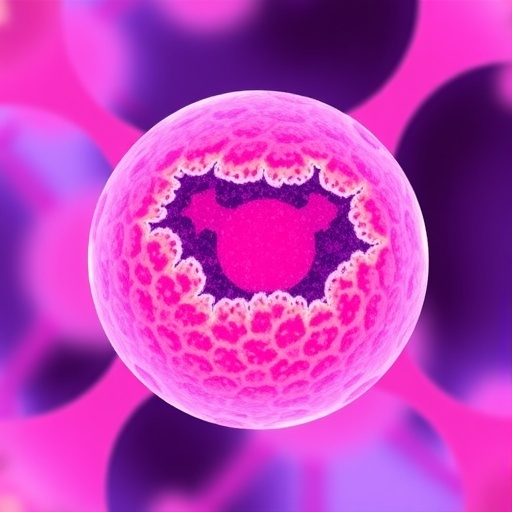
Polycystic ovary syndrome (PCOS) represents a multifaceted reproductive disorder that affects a significant proportion of women of reproductive age. The condition encompasses a broad spectrum of clinical manifestations, including irregular menstrual cycles, hirsutism, acne, and obesity, ultimately leading to far-reaching implications on metabolic health and reproductive capabilities. Recent research has increasingly turned its focus toward elucidating the underlying mechanisms of PCOS, particularly emphasizing the role of the ovarian microenvironment and its biochemistry. A forthcoming study from a group of researchers, led by Wang et al., sheds light on the intricate interplay of metabolites within follicular fluid and the implications for understanding PCOS pathogenesis.
The researchers embarked on a journey that incorporated cutting-edge techniques such as 16S ribosomal RNA (rRNA) sequencing and metabolomics to detail the microenvironmental modifications observed in the follicular fluid of women diagnosed with PCOS. This pioneering approach does not merely capture the hormonal profiles typically associated with PCOS but rather paints a comprehensive picture encompassing the metabolic state of the ovarian follicles. By leveraging the mechanistic insights gained from metagenomics and metabolomics, the team aims to identify specific molecular signatures that could shed light on how microenvironmental changes catalyze the onset of PCOS.
As numerous studies have shown, the composition of the follicular fluid can provide valuable insights into the health and functionality of the surrounding ovarian tissues. The approach by Wang et al. integrates this philosophy by examining not just hormone levels but also diverse metabolites that can reflect the overall metabolic health of the follicle. This enriched perspective may allow researchers to identify pivotal signals that could lead to the development or exacerbation of PCOS. With a detailed and comprehensive method, the study seeks to bridge the gap between metabolic dysregulation and traditional endocrinological models predominantly attributed to PCOS.
One of the critical components of this research involves analyzing the microbial communities present within the follicular fluid. This novel aspect garnered attention, especially as the association between the microbiome and various aspects of human health continues to unfold. The significance of gut microbiota is well-documented, but Wang et al. extend this investigation into the realm of reproductive health, demonstrating that alterations in microbiome composition may indeed influence ovarian function.
Metabolomics, the study of metabolites within a biological system, presents a revolutionary method for comprehensively examining the biochemical changes associated with health and disease. By utilizing high-resolution mass spectrometry and nuclear magnetic resonance spectroscopy, the researchers meticulously cataloged diverse metabolites in follicular fluid, seeking biomarkers that differentiate healthy individuals from those with PCOS. The insight garnered from such analyses lays the groundwork for identifying potential therapeutic targets and diagnostic markers.
The study further explores the relationship between the metabolic alterations and clinical manifestations of PCOS. By correlating metabolomic findings with clinical data, Wang et al. were able to identify specific metabolic pathways that are disrupted in patients with PCOS, linking them to well-characterized symptoms of the syndrome. This integrative methodology not only quantifies the biochemical disturbances associated with PCOS but also correlates them with the clinical outcomes experienced by patients.
A noteworthy aspect of this research involves the recognition that PCOS is not solely a reproductive issue; it is increasingly regarded as a metabolic disorder as well. The shifts in metabolite profiles within follicular fluid encapsulate the complexity of PCOS, highlighting the interconnectedness of reproductive and metabolic health. Findings from this study emphasize the necessity of a holistic view when addressing PCOS management, advocating for comprehensive treatment strategies that encompass metabolic health as part of patient care.
In the broader context of women’s health, understanding the microenvironment of the ovary and how it contributes to disorders like PCOS is paramount for developing effective interventions. Early identification of dysregulated metabolic profiles may allow healthcare providers to initiate preventative strategies, thus reducing the incidence or severity of PCOS manifestations. This preventive approach is particularly relevant as increased awareness of PCOS’s potential complications—including infertility, cardiovascular disorders, and insulin resistance—continues to rise.
Importantly, the study by Wang et al. aligns with a growing trend in medical research that aims to personalize medicine based on individual metabolic profiles. As technological advancements in metabolomics and genomics continue to evolve, there is a golden opportunity for healthcare providers to tailor interventions that are concordant with a patient’s specific metabolic makeup. Such precision medicine could revolutionize treatment protocols for those afflicted by PCOS and ultimately lead to enhanced quality of life.
Additionally, as more studies explore the significant public health implications of PCOS and its metabolic underpinnings, the need for comprehensive healthcare policies targeting women’s health becomes increasingly vital. By integrating findings from cutting-edge research, healthcare administrators have the opportunity to improve strategies for diagnosing and managing PCOS, amplifying awareness of the disorder and fostering interdisciplinary collaboration among healthcare providers.
In summary, Wang et al.’s exploration of the mechanisms underlying PCOS through the lens of the follicular fluid’s microenvironment stands as a testament to the power of modern science—melding traditional approaches with innovative technologies. With the momentum gathered through studies like this, the hope is to unveil the complexities of PCOS, ultimately leading to more effective management and treatment options. Not only does this research bring us closer to untangling the web of biomarkers associated with PCOS, but it also illuminates a pathway for future investigations into the nexus of ovarian health and metabolic disorders.
As the insights derived from this study ripple through the scientific community, there is an anticipatory fervor for the potential breakthroughs that may emerge from an enhanced understanding of PCOS. The implications of these findings extend not only to those directly affected by the syndrome but may also resonate within the broader field of reproductive medicine, inspiring future studies aimed at unraveling other multifactorial reproductive disorders. It exemplifies the necessity of an integrative approach to research—unearthing the intertwined, multifaceted aspects of health that collectively shape women’s reproductive experiences.
This groundbreaking research promises to fuel ongoing discussions surrounding PCOS and its treatment, emphasizing the urgency of addressing women’s health holistically. By recognizing the importance of the ovarian microenvironment and leveraging advanced technologies to uncover its secrets, the path toward more targeted therapies is illuminated, fostering hope for countless women grappling with the challenges posed by PCOS.
Subject of Research: Mechanisms of PCOS Induced by Microenvironmental Changes in Follicular Fluid.
Article Title: Exploration of the mechanism of PCOS induced by microenvironmental changes in follicular fluid based on 16 S rRNA and metabolomics.
Article References:
Wang, C., Zhao, H., Sibirny, A. et al. Exploration of the mechanism of PCOS induced by microenvironmental changes in follicular fluid based on 16 S rRNA and metabolomics. J Ovarian Res 18, 201 (2025). https://doi.org/10.1186/s13048-025-01781-5
Image Credits: AI Generated
DOI:
Keywords: PCOS, follicular fluid, 16S rRNA, metabolomics, women’s health, metabolic disorder, biomarkers, personalized medicine.