In a groundbreaking study published in BMC Cancer, researchers have unveiled the transformative potential of ultrasound texture analysis in diagnosing the diverse pathological types of primary testicular tumors in adults. This revelation could herald a new era in testicular cancer diagnostics, significantly refining treatment strategies and improving patient outcomes worldwide.
The clinical challenge in managing testicular tumors lies in their pathological heterogeneity—ranging from benign lesions like epidermoid cysts and sertoli-leydig cell tumors to aggressive malignant germ cell tumors and lymphomas. Traditionally, radical orchiectomy, the complete removal of the affected testicle, has been the standard approach due to the risks associated with tumor biopsy and the limitations of conventional imaging. However, this aggressive treatment often results in the unnecessary loss of testicles in patients harboring benign tumors, invoking an urgent need for more precise, non-invasive diagnostic modalities.
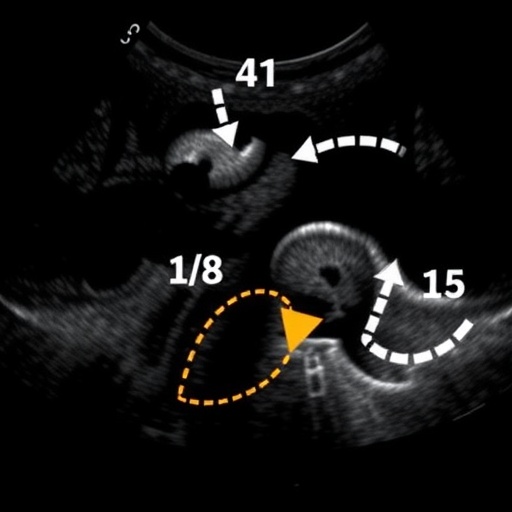
Conventional ultrasound has long been the frontline imaging technique for initial evaluation, but its capacity to differentiate between tumor types is limited by subjective interpretation and subtle echogenic distinctions. Ultrasound texture analysis, an advanced imaging technique that quantitatively evaluates the distribution and variation of grey-scale intensities within the tumor tissue, emerges as a revolutionary solution. By capturing the intricate patterns of tumor echoes and uniformity, texture analysis offers enhanced accuracy in reflecting the tumor’s underlying pathological architecture.
In this comprehensive retrospective investigation, a cohort of 86 patients presenting with a total of 89 testicular lesions underwent thorough evaluation with conventional ultrasound and texture analysis between February 2017 and June 2021. These patients were stratified into four distinct groups based on histopathological confirmation: epidermoid cysts, sertoli-leydig cell tumors, lymphomas, and malignant germ cell tumors. This stratification enabled a rigorous comparative analysis between imaging diagnoses and gold-standard pathological findings.
The results illuminated the limitations of conventional ultrasound alone, with sensitivity rates for detecting sertoli-leydig cell tumors and epidermoid cysts languishing at 40% and 22.2%, respectively. Similarly, lymphoma and malignant germ cell tumor detection rates were 15.8% and 19.0%, underscoring the pressing need for improved diagnostic methodologies. While specificities remained high, the low sensitivity of conventional ultrasound resulted in suboptimal diagnostic confidence and potential overtreatment.
The study’s focal innovation revolves around the application of nine quantitative texture feature parameters—minimum gray, maximum gray, standard deviation, skewness, contrast, sum average, difference variance, difference entropy, and dissimilarity—combined with patient age and tumor size metrics in a sophisticated binary logistic regression model. This multifactorial approach quantified the likelihood of each pathological classification, allowing for a nuancical diagnostic insight surpassing traditional methodologies.
Notably, receiver operating characteristic (ROC) analyses demonstrated remarkable diagnostic performance using this combined model. The area under the curve (AUC) values approached near perfection for several tumor types: 0.992 for sertoli-leydig cell tumors, 0.970 for epidermoid cysts, and 0.971 for lymphomas. Even malignant germ cell tumors, traditionally challenging to diagnose, achieved a commendable AUC of 0.809. Such robust discriminatory power translates into sensitivity and specificity rates exceeding 90% for most tumor categories when assessed by the joint diagnostic model.
Statistically significant improvements were observed when texture analysis was integrated into routine ultrasound assessments. This combined method yielded sensitivity, specificity, and overall accuracy rates sharply elevated beyond conventional ultrasound, providing clinicians with unparalleled diagnostic precision essential for personalized treatment pathways. Consequently, this technique promises to minimize unnecessary orchiectomy, particularly in patients harboring benign lesions, conserving testicular function and improving quality of life.
The implications of this study extend beyond technical innovation; they signal a paradigm shift in testicular cancer management. Preoperative differentiation of tumor pathology using non-invasive imaging can tailor surgical planning, informing clinical decisions that balance oncologic control with preservation of fertility and hormonal function. Particularly for younger male populations, this advancement holds profound significance.
Furthermore, this research underscores the potential of artificial intelligence and machine learning to be integrated in future ultrasound platforms, automating texture feature extraction and aiding radiologists in real-time diagnosis. Enhanced reproducibility and standardization of ultrasound texture parameters could foster multicenter collaborations and larger prospective trials, cementing the clinical utility of this novel imaging biomarker.
Despite the encouraging outcomes, the authors acknowledge certain limitations inherent to retrospective design and sample size constraints. Prospective validation in larger, diverse cohorts is warranted to corroborate these findings and refine predictive algorithms. Additionally, exploring texture analysis performance across different ultrasound equipment and operators will be crucial to establishing widespread applicability.
In sum, this pioneering study illuminates ultrasound texture analysis as a compelling adjunct to traditional imaging, dramatically enhancing the diagnostic landscape of primary testicular tumors. By leveraging detailed quantitative assessment of tumor echotexture alongside demographic and morphological data, this approach unlocks a new frontier in precision medicine—delivering tailored, effective care while safeguarding patient well-being.
Future directions may include integration of multimodal imaging data, such as elastography and contrast-enhanced ultrasound, to further amplify diagnostic accuracy. The convergence of radiomics and clinical oncology thus opens transformative opportunities for early, accurate tumor characterization with profound therapeutic impact.
Clinicians, radiologists, and oncologists alike will eagerly watch the evolution of this technology, which holds promise to reduce overtreatment, optimize surgical interventions, and ultimately improve survival and quality of life in men affected by testicular tumors worldwide.
Subject of Research: Ultrasound texture analysis in the pathological diagnosis of primary testicular tumors in adults.
Article Title: The value of ultrasound texture analysis in the diagnosis of pathological types of primary testicular tumours in adults.
Article References:
Yu, D., Xue, N. The value of ultrasound texture analysis in the diagnosis of pathological types of primary testicular tumours in adults. BMC Cancer 25, 1798 (2025). https://doi.org/10.1186/s12885-025-15232-3
Image Credits: Scienmag.com
DOI: 21 November 2025