In the remote expanses of East Sennar State in Sudan, a fascinating intersection of traditional medicine and contemporary healthcare is reshaping the battle against a devastating tropical disease—mycetoma. Mycetoma, a chronic granulomatous infection primarily affecting the skin and underlying tissues, has long posed significant health challenges in many arid and semi-arid regions. Despite advancements in medical science, many communities in Sudan still rely heavily on indigenous knowledge systems and traditional healing practices to manage this disabling condition. A groundbreaking qualitative exploration led by Elsheikh, Trueba, and Zaman has cast new light on this intricate relationship, revealing deeper insights into how local healers and conventional health services coexist in addressing mycetoma.
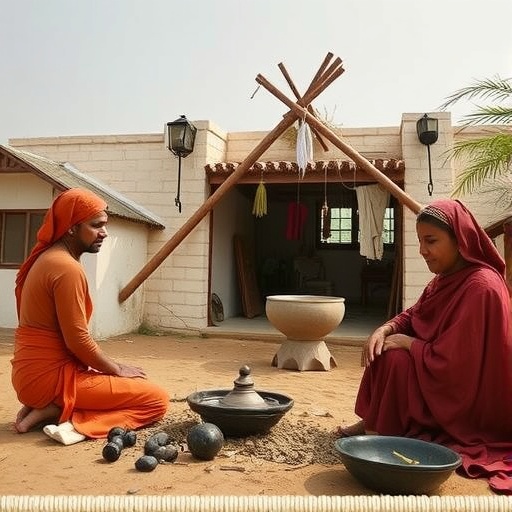
The study dives into the cultural paradigms and socio-economic realities that sustain traditional healing’s prominent role in mycetoma management within East Sennar. Historically relegated to the periphery of formal health systems, traditional medicine remains a foundational pillar in the lives of the Sudanese pastoral and agricultural populations. These methods encompass a variety of rituals, herbal remedies, and spiritual interventions, each embedded with centuries of empirical knowledge. Against the backdrop of limited access to modern healthcare facilities and the stigmatization often associated with mycetoma, traditional healers serve not only as caregivers but also as pivotal community figures who shape health-seeking behaviors.
Technically, mycetoma can be caused by both bacterial (actinomycetoma) and fungal (eumycetoma) pathogens, complicating diagnosis and treatment strategies. The coarse grains or granules discharged from lesions are diagnostic hallmarks. The disease progresses insidiously, leading to extensive tissue destruction, deformity, and disability if untreated. The management in biomedical settings involves prolonged courses of antifungal or antibacterial agents, surgical intervention, and often significant healthcare costs. However, in rural Sudan, the durability and accessibility of traditional healing emerge as pragmatic solutions when modern healthcare infrastructure is deficient or culturally incompatible.
One of the key revelations of this investigation is how local healers employ a rich pharmacopeia derived from native botanicals. These plant-based therapies, often prepared through maceration, decoction, or topical applications, demonstrate bioactive properties that merit pharmacological scrutiny. Moreover, the symbolic and therapeutic rituals embedded in treatment protocols might have psychosocial benefits that enhance patients’ perceived efficacy and adherence. The multifaceted approach of traditional medicine, blending physical, spiritual, and communal healing, offers a holistic model that is rarely accounted for in conventional disease management paradigms.
Importantly, the qualitative research illustrates the dynamic negotiations between traditional practitioners and biomedical health workers. While friction and mistrust persist in some instances, there are growing efforts towards integrative frameworks that respect indigenous knowledge while ensuring scientific rigor and patient safety. Local healthcare authorities are increasingly advocating for educational programs that bridge the knowledge gap, emphasizing collaborative treatment protocols that leverage the strengths of both systems to optimize therapeutic outcomes.
The study further elucidates how socio-cultural beliefs affect health-seeking timelines. Often, patients initially consult traditional healers for mycetoma symptoms, delaying biomedical intervention until disease progression accelerates. This delay unfortunately leads to more complex clinical presentations, necessitating aggressive pharmaceutical and surgical management. By understanding these cultural determinants, healthcare policies can be tailored to encourage early diagnosis and prompt treatment without alienating the traditional care networks that hold community trust.
A technological breakthrough in this context is the potential integration of diagnostic tools that can be operated in field settings accessible to both traditional healers and biomedical staff. Point-of-care molecular diagnostics or lateral flow assays, for instance, could facilitate early differentiation between fungal and bacterial mycetoma, enabling tailored treatment regimens. Empowering traditional practitioners with such tools through training could drastically improve patient referral patterns and reduce morbidity.
From an equity perspective, the complexity of mycetoma’s epidemiology demands culturally sensitive intervention models that address disparities in healthcare access. The East Sennar region exemplifies how intersecting issues of poverty, rurality, and cultural heritage influence health outcomes. The qualitative insights presented by Elsheikh and colleagues emphasize that to combat neglected tropical diseases effectively, strategies must go beyond biomedical solutions, incorporating community engagement, capacity building, and respect for indigenous systems.
The public health implications of these findings extend beyond mycetoma. They shed light on broader challenges encountered in global health when modern medicine encounters traditional practices. The lessons learned in Sudan resonate with initiatives worldwide seeking to harmonize pluralistic health approaches and foster sustainable healthcare delivery in underserved populations. Traditional healers, often marginalized in official health dialogues, could be pivotal allies if properly integrated and supported.
On the scientific frontier, further pharmacological validation of the herbal treatments employed by traditional healers offers promising avenues for novel antimycotic agents. As drug resistance and treatment failures persist, bio-prospecting ethnomedicinal plants could yield new compounds with unique modes of action. Collaborative research that respects the intellectual property rights of indigenous communities could foster ethical biomedical innovation and global health benefits.
The exploratory nature of the research has also highlighted a pressing need for structured training and certification programs for traditional healers. Standardizing safe practices and fostering dialogue with biomedical professionals would mitigate risks such as incorrect diagnosis, harmful interventions, and delayed referrals. Culturally competent health education campaigns aimed at villages may empower communities to make informed decisions about integrated care pathways.
Importantly, the psychological and social dimensions of mycetoma deserve further elaboration. Patients suffering from this disfiguring disease often encounter stigma, social isolation, and economic hardship. Traditional healing approaches that incorporate communal rituals may provide essential social support networks. Mental health services integrated alongside physical treatment could vastly improve quality of life for affected individuals.
This landmark qualitative study conducted in East Sennar State is a clarion call to rethink health intervention frameworks for neglected tropical diseases. By transcending the binary of traditional versus modern medicine, it advocates for synergistic models that recognize the validity and value of indigenous knowledge within scientific paradigms. Such integrative approaches hold immense promise for addressing complex health challenges in resource-limited environments.
In conclusion, Elsheikh, Trueba, and Zaman’s research provides a compelling account of the ongoing dialogue between tradition and innovation in managing mycetoma. Their findings underscore the necessity of culturally nuanced, scientifically informed, and community-driven health strategies. As global health efforts intensify in response to neglected diseases, embracing pluralistic healthcare models will not only improve outcomes but also uphold the dignity and heritage of affected populations.
Subject of Research: Traditional healing practices and their role in the management of mycetoma in East Sennar State, Sudan.
Article Title: Traditional healing and mycetoma management in East Sennar State (Sudan): a qualitative exploration.
Article References:
Elsheikh, M., Trueba, M. & Zaman, S. Traditional healing and mycetoma management in East Sennar State (Sudan): a qualitative exploration.
Int J Equity Health 24, 296 (2025). https://doi.org/10.1186/s12939-025-02641-w
Image Credits: AI Generated