In a groundbreaking study recently published in Nature Communications, researchers have unveiled the intricate genomic epidemiology of the monkeypox (mpox) virus during the unprecedented 2022 outbreak in New York City. This investigative work sheds light on the virus’s evolution and transmission dynamics, providing crucial insight into how the outbreak unfolded in one of the world’s most densely populated urban centers. By leveraging cutting-edge genomic sequencing and sophisticated phylogenetic analyses, this research offers an unprecedented window into the transmission chains and mutational landscape of the mpox virus.
The outbreak posed a unique challenge due to the virus’s previously rare occurrence outside endemic regions, combining factors such as international travel, urban density, and shifting social behaviors. Researchers from multiple institutions collaborated to sequence the viral genomes from clinical samples obtained during the height of the outbreak. This systematic approach enabled the identification of distinct viral lineages responsible for the observed infections, underscoring the complex epidemiology that had eluded traditional contact tracing methods.
At the heart of this study was the utilization of whole-genome sequencing technologies enabling real-time surveillance. Over 400 samples were sequenced, revealing subtle yet significant genetic variations across different viral isolates. This level of resolution was critical, as it allowed the team to reconstruct transmission networks and infer the temporal progression of the outbreak. Notably, the data indicated multiple introductions of the virus into New York City, challenging early assumptions of a single-source outbreak.
The research also pinpointed a spectrum of mutations accumulated during the outbreak, some of which potentially influence the virus’s infectivity and immune evasion capabilities. By employing comparative genomics, the study delineated these genetic shifts against the backdrop of previously known mpox virus genomes. The analysis suggested adaptive evolution, possibly driven by the intense transmission pressures within the urban sexual networks predominantly affected during this outbreak.
One of the most compelling findings pertained to the identification of superspreading events, which were implicated in accelerating viral dissemination. Genetic clusters revealed that particular subpopulations served as nodes facilitating rapid transmission, providing clarity on epidemiological patterns that were previously speculative. This genomic evidence reinforces the importance of targeted public health interventions to mitigate further spread in similar contexts.
Furthermore, this study highlighted the utility of integrating genomic data with epidemiological metadata, such as patient demographics, symptom onset dates, and behavior patterns. This integrative approach enabled a nuanced understanding of how social and biological factors intertwine in shaping outbreak dynamics. Insights gained here are anticipated to inform better outbreak response strategies, including contact tracing efficiency and vaccination prioritization.
Intriguingly, the research also addressed the question of viral persistence, with findings suggesting no evidence of significant viral reservoirs outside human hosts sustaining prolonged transmission chains. This aligns with the historical understanding of mpox but contrasts with concerns regarding potential animal reservoirs in urban settings. Such conclusions are pivotal for guiding surveillance efforts and resource allocation.
The team employed advanced phylogenetic modeling to trace the geographic origins of multiple viral introductions. The results implicated travel-related events, linking specific lineages to travel corridors between New York and other international hotspots. This aspect underscores the interconnected nature of modern pandemics and the role of global mobility in shaping local outbreak patterns.
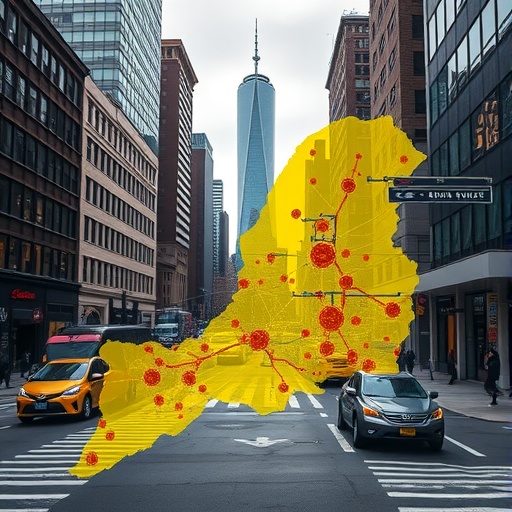
Moreover, the granular genomic data facilitated the tracking of viral spread within different boroughs of New York City, revealing heterogeneous transmission intensities. This spatial resolution is instrumental for public health authorities to deploy localized interventions rather than blanket measures, enhancing both efficacy and public compliance.
Crucially, the study’s findings have implications beyond mpox itself. They illustrate the transformative potential of genomic epidemiology as a core component of infectious disease surveillance, especially in metropolitan environments where traditional epidemiological tools might fall short. This work exemplifies how genomic data can rapidly elucidate transmission dynamics during outbreaks, leading to smarter, data-driven responses.
In response to the outbreak, public health responses evolved in real-time, with genomic surveillance guiding vaccination campaigns targeted at high-risk populations. The research highlights the importance of maintaining and expanding sequencing capacities, as early detection of viral evolution can preempt the emergence of variants with enhanced pathogenicity or transmission.
This study also contributes to the broader scientific understanding of poxvirus biology. Through detailed mutation mapping, researchers observed whether any genetic changes correlated with altered clinical manifestations or disease severity. While no conclusive links were found during this investigation, ongoing monitoring is recommended to detect any shifts that could affect clinical outcomes.
Beyond immediate public health benefits, this research sets a precedent for future outbreak preparedness. It underscores the necessity of collaborative networks that bridge clinical, genomic, and epidemiological expertise. The multidisciplinary framework employed here can serve as a blueprint for responding more effectively to emergent viral threats in complex urban landscapes.
In conclusion, the 2022 New York City mpox outbreak has been meticulously dissected through the lens of genomic epidemiology, revealing multifaceted viral evolutionary pathways and transmission dynamics. This study not only advances our understanding of mpox virus behavior in non-endemic regions but also exemplifies the critical role of genomics in modern outbreak response. As urban centers continue to face infectious disease threats, such integrative scientific approaches will be indispensable for safeguarding public health.
Subject of Research: Genomic epidemiology and transmission dynamics of the mpox virus during the 2022 outbreak in New York City.
Article Title: Genomic epidemiology of mpox virus during the 2022 outbreak in New York City.
Article References:
Akther, S., Su, M., Wang, J.C. et al. Genomic epidemiology of mpox virus during the 2022 outbreak in New York City. Nat Commun 16, 8354 (2025). https://doi.org/10.1038/s41467-025-60486-x
Image Credits: AI Generated