In a groundbreaking case report recently published, researchers explored the harrowing journey of a patient suffering from thalassemia who developed multiple brown tumors attributed to parathyroid adenoma. This intriguing interplay between thalassemia and parathyroid pathology, encapsulated within the findings of Liu et al., highlights various complexities regarding bone metabolism in individuals with hematological disorders. This case, identified through the innovative imaging method of ^18F-FDG PET/CT, underscores the critical role such technology plays in diagnosing and managing endocrine and calcium-related disorders.
Thalassemia, a hereditary blood disorder characterized by the abnormal formation of hemoglobin, has far-reaching implications not only for hematology but for overall patient health. Individuals affected by thalassemia often struggle with anemia, requiring frequent blood transfusions, which can lead to secondary complications. Among these, the development of osteodystrophy and related bone pathologies is not uncommon, posing significant challenges for both patients and healthcare providers. Liu et al.’s report exemplifies how these complications can manifest uniquely in different patients.
The phenomenon of brown tumors, or osteitis fibrosa cystica, is of particular interest as it relates to hyperparathyroidism. Brown tumors are not neoplastic but are instead a reactive bone lesion resulting from elevated levels of parathyroid hormone, typically leading to increased osteoclastic activity and subsequent bone resorption. In this case, the patient’s multiple brown tumors raised concerns that perhaps had previously gone undiagnosed, demonstrating the importance of differential diagnoses in similar cases.
The role of parathyroid adenoma in this context cannot be overstated. Parathyroid adenomas are benign tumors of the parathyroid glands that lead to hyperparathyroidism. This condition causes the release of excessive parathyroid hormone (PTH), significantly influencing calcium homeostasis and bone integrity. The development of such adenomas, particularly in patients with chronic conditions like thalassemia, necessitates vigilant monitoring and appropriate imaging studies to gauge the extent of skeletal complications.
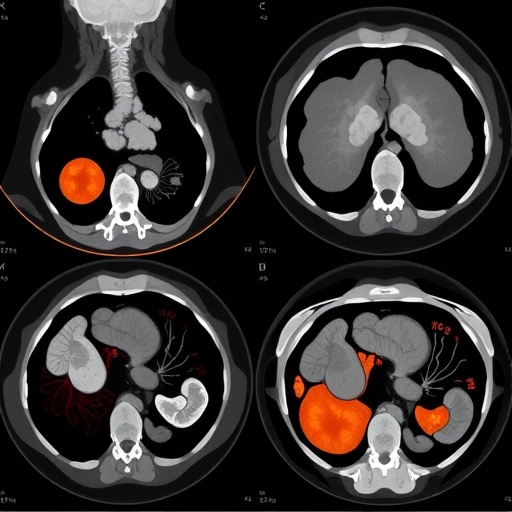
The application of ^18F-FDG PET/CT in this report marks a significant advance in assessing metabolic bone disease. This imaging technique allows for the visualization of metabolic activity in bone lesions, differentiating between malignant processes and those that are reactive, such as the brown tumors seen in this patient. The increased uptake of ^18F-FDG in these lesions indicates heightened metabolic activity, further prompting investigations into the underlying pathophysiology.
A detailed analysis of the imaging findings revealed multiple areas of increased uptake in the skeletal framework of the patient. The presence of these lesions prompted a reevaluation of the patient’s overall management strategy, highlighting the essential coordination between endocrinologists, hematologists, and radiologists. Such multidisciplinary approaches are vital in formulating treatment plans that address both the primary hematological condition and its associated endocrine sequelae.
The complexity of managing a patient with thalassemia who also exhibits signs of secondary hyperparathyroidism emphasizes the need for a personalized treatment pathway. In many instances, the surgical removal of the parathyroid adenoma may be indicated to alleviate the symptoms of hyperparathyroidism while simultaneously reducing the risk of further skeletal complications. This surgical intervention can lead to significant improvements in patient quality of life and bone health, as evidenced in previous studies.
Furthermore, the implications for clinical practice stemming from Liu et al.’s case report reflect a growing awareness of the importance of endocrine evaluations in patients with chronic hematological disorders. Routine monitoring of calcium and PTH levels should be considered as part of the broader management plan for individuals suffering from thalassemia, especially given their increased vulnerability to metabolic bone diseases.
As healthcare professionals navigate the complexities of treating such multifaceted conditions, continuous education and vigilance in monitoring for unanticipated complications are paramount. Case studies like the one presented by Liu et al. provide invaluable insights into the nuances of patient care, encouraging clinicians to think broadly about the potential systemic implications of localized conditions.
In conclusion, the case report raises critical questions regarding the intersection of hematological and endocrine health. Brown tumors arising from parathyroid adenoma in a thalassemia patient illustrate the intricate web of interconnected physiological processes at play. This highlighted overlap serves as an urgent call to action for researchers and clinicians alike, emphasizing the necessity for integrated medical care in addressing chronic illnesses.
With the advancements in imaging technology and a deepening understanding of these conditions, the medical community is better equipped to diagnose and manage complex cases. Such revelations not only advance our knowledge but also serve to improve patient outcomes, paving the way for future research and clinical guidelines that take into account the multifactorial nature of such medical anomalies.
This case report stands as a reminder of the importance of a cohesive approach in medicine, where understanding one condition can unlock new pathways to treat and manage others. As more cases come to light, the landscape of our understanding will continue to evolve, providing hope for patients grappling with the challenges of chronic disease.
As we look to the future, the collaboration between different specialties in healthcare will be crucial in unraveling the interconnectedness of diseases. Sharing knowledge and insights fosters a landscape where innovative treatments can flourish, ultimately enhancing patient care across the spectrum of medical disciplines.
Subject of Research: Multiple brown tumors caused by parathyroid adenoma in a thalassemia patient.
Article Title: Multiple brown tumors caused by parathyroid adenoma identified by ^18F-FDG PET/CT in a patient with thalassemia: a case report.
Article References:
Liu, XF., Xiang, ZY., Zhu, LB. et al. Multiple brown tumors caused by parathyroid adenoma identified by 18F-FDG PET/CT in a patient with thalassemia: a case report.
BMC Endocr Disord (2025). https://doi.org/10.1186/s12902-025-02078-w
Image Credits: AI Generated
DOI: 10.1186/s12902-025-02078-w
Keywords: Thalassemia, Brown Tumors, Parathyroid Adenoma, ^18F-FDG PET/CT, Hyperparathyroidism, Bone Metabolism, Multidisciplinary Care.