In the evolving landscape of cancer immunology, tertiary lymphoid structures (TLSs) have garnered significant attention for their role in orchestrating antitumor immune responses across a variety of malignancies. These ectopic lymphoid formations, arising within chronically inflamed tissues and tumors, function analogously to secondary lymphoid organs, facilitating localized immune cell interactions that potentiate tumor surveillance and elimination. While TLSs have been extensively characterized in cancers such as melanoma, lung, and breast carcinomas, their presence and prognostic implications in pediatric liver malignancies, especially hepatoblastoma (HB), remain enigmatic. A groundbreaking study published in Pediatric Research by Sun et al. (2025) now illuminates the landscape of TLS in HB, unveiling novel insights into their distribution, prognostic value, and the intricate interplay with the tumor immune microenvironment following neoadjuvant chemotherapy.
Hepatoblastoma stands as the most common liver malignancy in children, often necessitating multimodal treatment strategies that include chemotherapy and surgical resection. Despite therapeutic advances, clinical outcomes vary widely, with a subset of patients exhibiting relapse or resistance. Understanding the immunological milieu within HB is essential to enhance prognostication and develop immune-targeted therapies. In this context, the study by Sun and colleagues pioneers the exploration of TLSs within the HB tumor microenvironment, interrogating not only their spatial configuration but also their potential as predictive biomarkers post-chemotherapy.
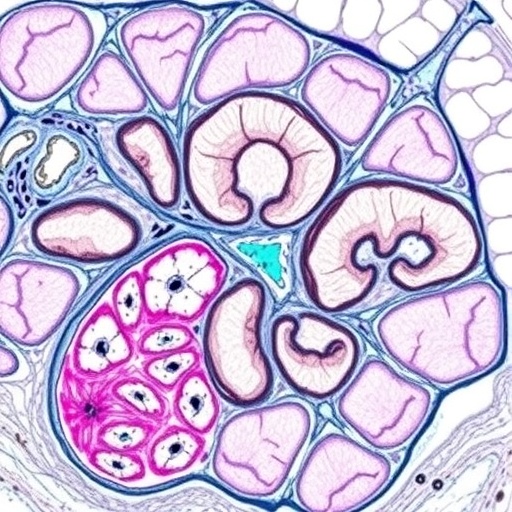
The research team undertook a comprehensive histopathological analysis of tumor specimens from HB patients treated with neoadjuvant chemotherapy. Employing state-of-the-art immunohistochemical techniques and spatial profiling, the authors identified TLSs categorized by their maturity and cellular architecture. This stratification allowed for the evaluation of TLS density and localization relative to tumor parenchyma and stromal compartments. Remarkably, the study demonstrated a heterogeneous distribution of TLSs across samples, with a predilection for peritumoral regions, suggesting a dynamic immunological niche fostered by therapeutic interventions.
Delving deeper into the prognostic ramifications, the investigators correlated TLS density with clinical outcomes, revealing that high TLS prevalence portended significantly improved survival rates and reduced recurrence in HB patients. This association underscores the functional relevance of TLSs as hubs of antitumor immunity. The ability of TLSs to sustain intratumoral lymphocyte activation and facilitate antigen presentation likely underpins their favorable impact on prognosis. Such findings position TLSs as not merely passive histological curiosities but active players in cancer control, holding tangible prognostic and therapeutic implications.
Beyond mere enumeration, Sun et al. dissected the cellular and molecular constituents of TLSs within HB, unveiling a complex ecosystem intertwining B cells, T follicular helper (Tfh) cells, dendritic cells, and stromal fibroblasts. The presence of germinal center-like structures within mature TLSs attests to ongoing affinity maturation and clonal expansion of B cells, processes integral to adaptive antitumor immunity. Concomitantly, subsets of cytotoxic CD8+ T cells and regulatory T cells orchestrate a delicate immune balance, influencing tumor progression or regression. Understanding these finely tuned interactions provides a roadmap for immunomodulatory therapies aiming to enhance TLS functionality.
Intriguingly, the study sheds light on how neoadjuvant chemotherapy modulates the tumor immune microenvironment in HB, influencing TLS development and maintenance. Chemotherapeutic regimens traditionally viewed as immunosuppressive may paradoxically prime the immune milieu by inducing immunogenic cell death and releasing tumor antigens. This immunogenic remodeling presumably facilitates TLS neogenesis, augmenting local immune surveillance and potentiating long-term tumor control. These insights recalibrate perspectives on combining chemotherapy with immunotherapy, advocating for rational sequencing and synergy.
Technological advancements fueled the precision of the study’s spatial immunophenotyping. Multiplex immunohistochemistry allowed simultaneous visualization of multiple immune markers within TLSs, while computational pathology algorithms quantified TLS density with unprecedented accuracy. Such methodologies enable robust correlation between histological features and clinical data, paving the way for integrating TLS assessment into diagnostic workflows. Future integration with single-cell RNA sequencing and spatial transcriptomics could unravel the functional states of TLS-resident immune cells, enhancing not only prognostication but also personalized therapeutic stratification.
The elucidation of TLSs in HB also invites comparisons with other malignancies where TLS presence correlates with response to immune checkpoint blockade therapies. Given the relative paucity of immunotherapy options in pediatric oncology, these findings open prospective avenues for implementing TLS-based biomarkers to identify HB patients who might benefit from immune-based interventions. Additionally, engineering strategies to induce TLS neogenesis or enhance their immunostimulatory capacity could revolutionize treatment paradigms, contributing to more durable remissions and better quality of life.
From a translational standpoint, the study cautions against oversimplified interpretations of TLS presence, emphasizing the need to consider TLS maturity and spatial context. Immature TLSs, lacking organized germinal centers, might confer different immunological impacts compared to their mature counterparts. Furthermore, TLSs located intratumorally versus peritumorally may engage in distinct cellular dialogues, influencing their effectiveness in tumor suppression. These nuanced distinctions necessitate standardized criteria for TLS evaluation and underscore the complexity of tumor-immune interactions.
Sun et al.’s research also contemplates the mechanistic underpinnings guiding TLS formation in HB. Chronic inflammation within the tumor microenvironment, sustained by cytokine gradients such as lymphotoxin α/β and chemokines like CXCL13, orchestrates lymphoid neogenesis. The interplay of stromal fibroblasts and endothelial cells expressing vascular cell adhesion molecule-1 (VCAM-1) further scaffolds TLS architecture. Deciphering these molecular cues offers potential targets to manipulate TLS dynamics therapeutically, enhancing local antitumor immunity.
Broader implications of this study resonate beyond HB, highlighting the universality of TLS-mediated immune regulation in cancer biology. As our comprehension of tumor immunology deepens, recognizing the cellular ‘hotspots’ like TLSs that concentrate immune effector functions becomes pivotal. Clinicians and researchers alike must integrate these immune structures into diagnostic and therapeutic frameworks, shifting from tumor-centric models to a more holistic approach encompassing the immune microenvironment.
Notably, this investigation underscores the criticality of timing in analyzing tumor-immune landscapes. Assessing TLS presence post-chemotherapy reveals the treatment’s influence on immune remodeling, a parameter potentially obscured in naive tumors. Consequently, dynamic monitoring of TLS evolution during treatment courses could serve as a biomarker for therapeutic efficacy, enabling adaptive treatment modifications that optimize patient outcomes.
Scientifically, the study prompts intriguing questions ripe for future exploration: What governs the balance between protumor and antitumor immune elements within TLSs in HB? Can TLS-targeted therapies synergize with conventional chemotherapy to eradicate minimal residual disease? How does the pediatric immune system’s unique features influence TLS formation and function compared to adults? Addressing these inquiries will undoubtedly propel the frontier of pediatric cancer immunotherapy.
In conclusion, the landmark study by Sun and colleagues revolutionizes our understanding of tertiary lymphoid structures in hepatoblastoma, demonstrating their critical role as prognostic biomarkers and immune modulators in the post-chemotherapy setting. This work bridges a significant knowledge gap, setting the stage for integrating TLS assessment into HB clinical management. As the nexus between tumor cells and immune effectors sharpens, harnessing the power of TLSs may unlock transformative advances in pediatric oncology, ultimately translating scientific discovery into life-saving therapies.
Subject of Research: The presence, distribution, and prognostic significance of tertiary lymphoid structures in hepatoblastoma following neoadjuvant chemotherapy.
Article Title: Density of tertiary lymphoid structures predict clinical outcome in hepatoblastoma.
Article References:
Sun, R., Liu, Z., Zhang, Y. et al. Density of tertiary lymphoid structures predict clinical outcome in hepatoblastoma. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04210-x
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41390-025-04210-x
Keywords: Hepatoblastoma, tertiary lymphoid structures, tumor immune microenvironment, neoadjuvant chemotherapy, pediatric oncology, antitumor immunity, prognostic biomarkers, immunotherapy.