A groundbreaking study recently presented at the International Stroke Conference 2026 by the American Heart Association unveils promising advances in the therapeutic management of acute ischemic stroke. The research focuses on patients suffering non–large vessel occlusion ischemic strokes—a subtype of stroke where blood clots obstruct smaller cerebral arteries—yet retaining salvageable brain tissue, thereby opening a critical therapeutic window beyond the traditionally narrow timeframe.
This investigation rigorously evaluates the efficacy and safety profile of intravenous tenecteplase, a genetically modified variant of human tissue plasminogen activator (tPA), notable for its longer half-life and enhanced fibrin specificity relative to alteplase, the current gold standard thrombolytic agent. The study administered tenecteplase within an extended time frame of 4.5 to 24 hours post-stroke onset, a period generally considered beyond the usual acute intervention window.
Intravenous thrombolysis aims to restore cerebral blood flow by enzymatically dissolving the offending thrombus, thereby curbing ischemic damage and enhancing functional recovery. The extended therapeutic window explored here is significant; it challenges prevailing dogma that limits thrombolytic intervention to within 4.5 hours post-symptoms, potentially broadening eligibility and improving outcomes in a wider patient population.
Results demonstrated that tenecteplase administration within this delayed window significantly increased the probability of patients achieving an excellent functional outcome at 90 days, as measured by widely validated neurological scales. This functional recovery suggests meaningful restoration of neurological function and quality of life, a paramount goal in stroke therapeutics that transcends mere survival.
Nonetheless, the study uncovers a critical safety consideration—patients receiving tenecteplase exhibited a heightened risk of symptomatic intracranial hemorrhage (sICH), a potentially catastrophic bleeding complication within the brain parenchyma. The intricate balance between effective clot dissolution and hemorrhagic risk underlies the delicate pathophysiology of thrombolytic therapy.
Mechanistically, tenecteplase’s enhanced fibrin affinity facilitates targeted thrombolysis, yet this potent fibrinolytic activity may also compromise vascular integrity, particularly in ischemically vulnerable brain tissue. This paradox underscores the necessity of stringent patient selection and meticulous monitoring during therapy administration.
The study’s findings illuminate novel clinical implications for neurovascular specialists and stroke care practitioners, indicating that tenecteplase could become a viable alternative to traditional thrombolytics, especially in patients presenting outside the conventional therapeutic window—provided the bleeding risks are judiciously managed.
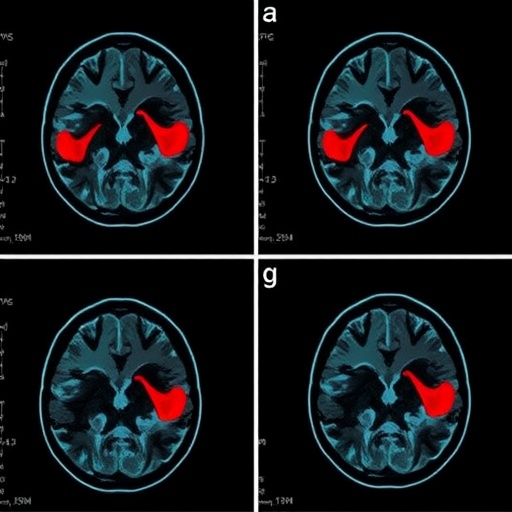
Advancements in neuroimaging to identify salvageable brain tissue, such as perfusion-diffusion MRI mismatch or CT perfusion techniques, have been pivotal. By refining patient selection criteria to those with potentially reversible ischemic penumbra, clinicians can tailor thrombolytic therapy more effectively, maximizing benefits while limiting adverse events.
Furthermore, the pharmacokinetic advantages of tenecteplase—increased resistance to plasminogen activator inhibitor-1 and reduced systemic clearance—may enhance its therapeutic utility. These factors enable single bolus administration, improving ease of use in emergency settings and potentially expediting reperfusion compared to continuous infusion regimens.
Clinical adoption of extended-window thrombolysis necessitates robust protocols, interdisciplinary coordination, and comprehensive patient education on recognizing delayed stroke symptoms and seeking urgent care. Health systems must adapt to these evolving paradigms to optimize outcomes across diverse clinical scenarios.
It is imperative that future research addresses the stratification of hemorrhagic risks associated with tenecteplase, exploring adjunctive neuroprotective strategies or dosing modifications to mitigate intracranial bleeding while preserving thrombolytic efficacy. Multicenter randomized controlled trials with larger cohorts are warranted to consolidate these preliminary findings.
This landmark study not only challenges existing treatment time constraints but also catalyzes a paradigm shift in acute ischemic stroke management, underscoring the progressive harnessing of molecularly engineered therapeutics to reconcile efficacy with safety in complex cerebrovascular interventions. The translation of such scientific insights into clinical practice could profoundly impact mortality and morbidity associated with stroke worldwide.
Correspondence regarding this pivotal research can be directed to Dr. Junwei Hao, MD, PhD, providing an access point for scientific dialogue and collaboration aimed at refining and expanding the clinical applications of tenecteplase in stroke care. The study is published in the esteemed journal JAMA, ensuring rigorous peer-review and dissemination within the global medical community.
The emerging narrative from this research encapsulates the relentless quest to extend functional recovery for stroke victims, entwining molecular innovation, advanced diagnostic imaging, and nuanced clinical judgement. As stroke remains a leading cause of long-term disability worldwide, these developments kindle hope for enhanced therapeutic interventions tailored to individual patient profiles.
Subject of Research: Therapeutic efficacy and safety of intravenous tenecteplase in non–large vessel occlusion acute ischemic stroke patients with salvageable brain tissue, administered beyond the conventional thrombolytic window.
Article Title: Information not provided
News Publication Date: Information not provided
Web References: Not available
References: (doi:10.1001/jama.2026.0210)
Image Credits: Not available
Keywords: Cerebrovascular disorders, Medical treatments, Brain tissue, Bleeding, Risk factors, Health care, Necrosis, Symptomatology