Recent research has delved into the intricate world of immunology and its potential implications for cancer therapy, focusing specifically on the role of Cathepsin S. This study elucidates how Cathepsin S governs interleukin-7-mediated anti-tumor immunity, offering promising insights into its effectiveness against oral cancer. The findings have sparked discussions in the scientific community, highlighting the urgent need for innovative approaches in cancer treatment protocols.
Interleukin-7 is a crucial cytokine that plays a significant part in the development and maintenance of T-cells, integral components of the adaptive immune system. By ensuring that immune cells are adequately equipped to combat cancer cells, interleukin-7 emerges as a potential therapeutic agent. Its role in modulating the immune response makes it a focal point of the investigation presented in the recent study.
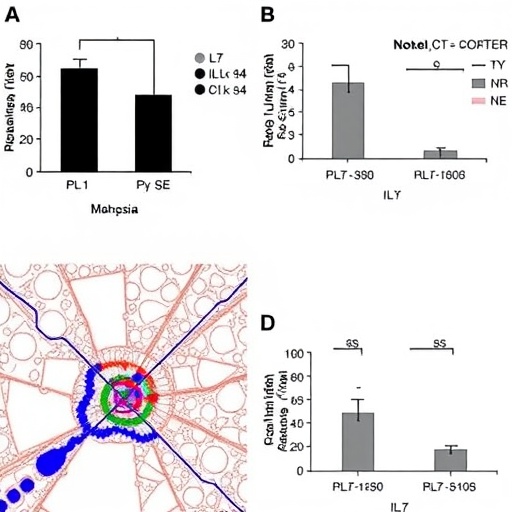
The researchers—led by Chang, YC., Chen, SJ., and Chen, SH.—focused on understanding how Cathepsin S regulates the immune response triggered by interleukin-7. This regulation is pivotal for ensuring that immune cells can effectively recognize and eliminate tumor cells. The findings underscore how aberrations in this pathway can lead to diminished anti-tumor immunity, thereby facilitating tumor growth and progression.
One of the significant observations from the research is how the modulation of Cathepsin S can enhance the efficacy of interleukin-7 in promoting immune responses against tumors. The study revealed that targeted manipulation of Cathepsin S levels could augment T-cell activation and proliferation. This presents a dual advantage: not only does it boost the body’s natural defenses, but it also provides a less invasive alternative to traditional cancer therapies, which often entail severe side effects.
The research also examined how Cathepsin S expression varies in different cancer contexts, particularly in oral cancer. The results indicated that higher levels of Cathepsin S correlate with more aggressive tumor phenotypes and poorer patient outcomes. This correlation suggests that Cathepsin S may serve as a biomarker for cancer severity and could guide therapeutic decisions in clinical settings.
Moreover, the study introduced novel methodologies to assess Cathepsin S activity, which could pave the way for developing targeted therapeutic strategies. This innovative approach could facilitate more precise interventions, allowing for personalized medicine to take center stage in cancer treatment. By carefully modulating Cathepsin S levels, clinicians may optimize the effects of interleukin-7, tailoring therapies to maximize patient outcomes.
The implications of this research extend beyond oral cancer. By understanding the broader role of Cathepsin S in interleukin-7-mediated immunity, researchers may uncover similar pathways in various cancers. This could significantly influence how oncologists approach treatment, potentially leading to new combinations of therapies that exploit the immune system to fight cancer more effectively.
Furthermore, the convergence of immunology and oncology is exemplified by these findings. The study reinforces the importance of the immune system in combating cancer and highlights the pressing need for more research in this area. As the complexity of the immune response becomes better understood, new opportunities arise for developing cutting-edge therapies that harness the body’s natural defenses.
The role of Cathepsin S in cancer biology is a burgeoning area of study, with implications that could change the therapeutic landscape. The study’s insights into molecular interactions within the tumor microenvironment challenge existing therapeutic paradigms, pointing towards a more integrated approach that considers both the tumor and the immune system.
In the wake of these findings, questions arise regarding how to implement these strategies in clinical practice. Increased emphasis on research translating laboratory findings into actionable therapies will be paramount. Therapies based on these insights could potentially revolutionize treatment options available to patients, making them safer and more effective.
As the scientific community collectively embraces these advancements, there will be an increasing need for collaboration across disciplines. Immunologists, oncologists, and drug developers must work together to explore the full potential of these findings. Such interdisciplinary efforts can accelerate the translation of knowledge from bench to bedside, ultimately improving patient care.
In conclusion, the research highlights an exciting frontier in cancer treatment: the intersection of immune modulation and targeted therapy. By unraveling the regulatory mechanisms surrounding Cathepsin S and interleukin-7, the study lays the groundwork for future innovations. Given the growing burden of cancer globally, these explorations are of utmost importance, as they could lead to new standards of care that encourage better survival rates and enhanced quality of life for patients diagnosed with this devastating disease.
The potential therapeutic implications of these findings cannot be overstated. As research continues to unveil the complexities of immune responses in cancer, the hope is to develop strategies that not only increase survival rates but also empower patients by minimizing their treatment burden.
In summary, the synthesis of data regarding Cathepsin S regulation in interleukin-7-mediated anti-tumor immunity signals a pivotal moment in cancer research. This study elevates our understanding of the immune system’s role in cancer progression, spotlighting the need for continued inquiry and collaboration in this vital area of study.
Subject of Research: Cathepsin S regulation in interleukin-7-mediated anti-tumor immunity
Article Title: Unraveling Cathepsin S regulation in interleukin-7-mediated anti-tumor immunity reveals its targeting potential against oral cancer.
Article References:
Chang, YC., Chen, SJ., Chen, SH. et al. Unraveling Cathepsin S regulation in interleukin-7-mediated anti-tumor immunity reveals its targeting potential against oral cancer.
J Biomed Sci 32, 69 (2025). https://doi.org/10.1186/s12929-025-01154-6
Image Credits: AI Generated
DOI: 10.1186/s12929-025-01154-6
Keywords: Cathepsin S, interleukin-7, anti-tumor immunity, oral cancer, immunotherapy, targeted therapy, T-cells, cytokine, personalized medicine.