In a promising advancement for breast cancer therapeutics, researchers have uncovered a potent synergy between Tanshinone IIA, a bioactive compound derived from traditional Chinese medicine, and olaparib, a well-known PARP inhibitor, in inducing apoptosis in triple-negative breast cancer (TNBC) cells. The study, recently published in Medical Oncology, explores this combination’s efficacy across both BRCA-proficient and BRCA-deficient TNBC cell lines, offering new hope for tackling one of the most aggressive and treatment-resistant subtypes of breast cancer.
Triple-negative breast cancer, characterized by the absence of estrogen, progesterone, and HER2 receptors, accounts for approximately 15-20% of breast cancer cases. Its aggressive nature and lack of targeted therapies make treatment particularly challenging, often relegating options to conventional chemotherapy with limited success. In this landscape, PARP inhibitors like olaparib have emerged as targeted therapies, especially effective in cancers harboring BRCA1 or BRCA2 mutations due to their role in DNA repair pathways. However, these inhibitors show limited efficacy in BRCA-proficient TNBC, necessitating novel strategies to extend their clinical utility.
The current investigation centers on Tanshinone IIA, a diterpene quinone isolated from Salvia miltiorrhiza (Danshen), known for its anti-inflammatory, antioxidant, and antineoplastic properties. Its involvement in modulating apoptosis and cell cycle regulation has piqued interest in oncology, though its combinatorial potential with existing chemotherapeutics remains underexplored. Here, the researchers probe whether Tanshinone IIA can potentiate the pro-apoptotic effects of olaparib, thereby enhancing therapeutic outcomes in TNBC cells regardless of BRCA status.
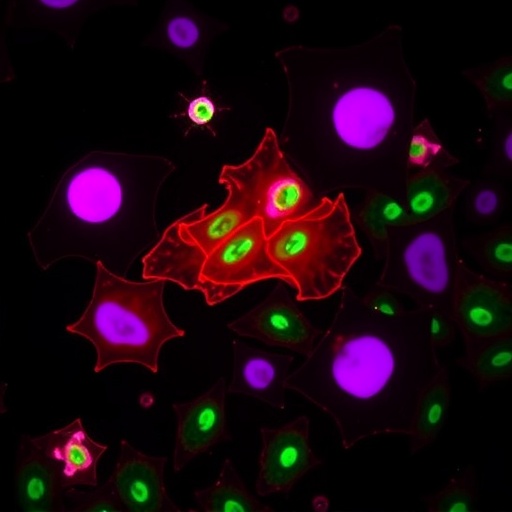
Utilizing in vitro cell culture assays, the research team treated BRCA-proficient and BRCA-deficient triple-negative breast cancer cell lines with varying concentrations of Tanshinone IIA and olaparib, both as monotherapies and in combination. Apoptosis rates, cell viability, and molecular markers associated with DNA damage and repair were meticulously quantified. The results strikingly demonstrated that combined treatment synergistically increased apoptotic cell death far beyond additive effects seen when each agent was used independently.
Mechanistically, the synergy appears to hinge upon Tanshinone IIA’s ability to exacerbate DNA damage and disrupt cellular repair pathways, thereby sensitizing cells to PARP inhibition. Particularly noteworthy was the activation of the intrinsic mitochondrial apoptosis pathway, evident from increased cytochrome c release and caspase cascade activation. Furthermore, the combination impaired homologous recombination repair efficiency, indicated by diminished RAD51 foci formation, an effect significant in both BRCA-proficient and deficient contexts.
Complementary Western blot analyses revealed that Tanshinone IIA treatment decreased expression of anti-apoptotic proteins such as Bcl-2 while upregulating pro-apoptotic Bax. This shift in the apoptotic balance, coupled with olaparib’s inhibition of PARP-mediated DNA repair, creates a metabolic and genomic environment hostile to cancer cell survival. Importantly, the combination strategy mitigated potential drug resistance mechanisms, a persistent challenge with monotherapies.
The implications of these findings are notably significant for the clinical management of TNBC. By extending the applicability of PARP inhibitors to a broader patient subset through combination with Tanshinone IIA, this approach could revolutionize current therapeutic paradigms. The dual targeting of DNA repair systems and apoptotic pathways offers a compelling rationale for subsequent preclinical animal studies and, ultimately, human clinical trials.
Notably, the study also evaluated the cytotoxicity profile of the combined treatment in non-cancerous mammary epithelial cells. Encouragingly, the synergy selectively targeted malignant cells with minimal toxicity to normal cells, suggesting potential for a favorable therapeutic index. This specificity is critical for minimizing adverse effects and improving patient quality of life during cancer treatment regimens.
The research team further explored signaling cascades modulated by the combination treatment, identifying inhibition of the NF-κB and PI3K/AKT pathways, known contributors to cancer cell survival and proliferation. Such multi-layered interference not only prompts apoptosis but also hinders metastatic potential, underscoring an additional benefit of this therapeutic approach.
While the study primarily focused on molecular and cellular responses in controlled in vitro settings, the authors emphasize the necessity of expanding into in vivo models that mimic the complex tumor microenvironment, immune interactions, and pharmacokinetic profiles. These forthcoming investigations are crucial to validate efficacy, safety, and dosing strategies that could streamline bench-to-bedside translation.
The integration of traditional natural compounds such as Tanshinone IIA with modern targeted agents exemplifies a burgeoning trend in oncology to revisit ethnopharmacology for novel drug candidates within combinatorial frameworks. The leveraging of such synergistic partnerships holds promise not only for breast cancer but also for other malignancies marked by DNA repair deficiencies and therapeutic resistance.
In summary, this study delineates a compelling new avenue in the fight against triple-negative breast cancer, demonstrating that Tanshinone IIA robustly enhances the apoptotic effect of the PARP inhibitor olaparib in both BRCA-proficient and -deficient TNBC cells. The mechanistic insights into DNA damage accumulation, repair inhibition, and apoptosis induction furnish valuable directions for future clinical development. As oncologists grapple with the heterogeneity and aggressiveness of TNBC, such innovative combination therapies could shift treatment paradigms and improve prognoses for many patients worldwide.
With ongoing advances, the therapeutic landscape of breast cancer is evolving rapidly, with research such as this exemplifying how natural compounds can be harnessed to amplify the efficacy of existing drugs. The dual assault on cancer cell DNA integrity and survival signaling presents a multidimensional strategy that may overcome the limitations of monotherapy. If validated in clinical settings, Tanshinone IIA and olaparib co-therapy can become a vital option in personalized cancer care.
As the scientific community continues to dissect the intricate mechanisms behind TNBC and its resistance strategies, integrative approaches combining molecular targeted agents and phytochemicals are poised to redefine the future of oncologic therapeutics. This study illuminates one such promising path, offering renewed optimism against a formidable disease.
Subject of Research: The synergistic anticancer effects of Tanshinone IIA combined with the PARP inhibitor olaparib in treating BRCA-proficient and -deficient triple-negative breast cancer cells.
Article Title: Tanshinone IIA is synergistic with the PARP inhibitor olaparib in inducing BRCAs-proficient and -deficient triple-negative breast cancer cell apoptosis.
Article References: Liu, Q., Zhou, Q., Yang, X. et al. Tanshinone IIA is synergistic with the PARP inhibitor olaparib in inducing BRCAs-proficient and -deficient triple-negative breast cancer cell apoptosis. Med Oncol 42, 419 (2025). https://doi.org/10.1007/s12032-025-02968-y
Image Credits: AI Generated