A groundbreaking study conducted collaboratively by the University of Cambridge and Bournemouth University has shed new light on the alarming rates of suicide among autistic individuals, revealing systemic failures and psychological burdens that exacerbate suicidal ideation and attempts within this community. This seminal research, published in the journal Autism in Adulthood, represents the largest survey to date examining the intersection of autism and suicide, involving nearly 1,400 autistic participants, predominantly from the United Kingdom. The findings provide an unprecedented window into the psychological struggles and institutional barriers facing autistic people, particularly emphasizing the roles of loneliness, hopelessness, and feelings of worthlessness as critical catalysts in suicidal experiences.
Central to the study’s revelations is the disproportionate vulnerability of autistic women and gender minorities, including transgender individuals, who faced significantly greater difficulties accessing necessary mental health and social support services. These service access challenges correlate strongly with increased suicide attempts, signaling profound systemic inequalities and deficiencies in health infrastructure. Lead researcher Dr. Rachel Moseley, Principal Academic in Psychology at Bournemouth University, candidly acknowledged the gravity of these statistics, noting that while suicide attempt rates among non-autistic populations hover around one in thirty-seven, approximately one in four autistic individuals report having attempted suicide at some point in their lives—a statistic that is both harrowing and indicative of a public health crisis.
The data underscore a psychological landscape marred by traumatic early experiences, especially during school years where many participants reported victimization, inadequate support, and bullying, experiences which seeded long-term emotional distress. This toxic environment often perpetuated into adulthood, manifesting in difficulties securing and maintaining employment, social isolation, and the exacerbation of mental health challenges. Participants frequently described the health and social care systems as “inconsistent and unpredictable,” compounding their hardship. Furthermore, the structural challenges posed by the welfare benefits system—a system participants characterized as “demeaning” and “cruel”—fostered pervasive feelings of being a burden to family and society, intensifying despair.
Professor Sir Simon Baron-Cohen, Director of the Autism Research Centre at Cambridge University and senior author of the study, framed these findings in a broader societal context. He emphasized that many autistic people feel marginalized and rejected by a world that fails to accommodate their needs, lacking equitable access to fundamental determinants of mental well-being such as tailored healthcare, appropriate social services, and inclusive education or employment opportunities. This marginalization translates directly into psychological distress, social alienation, and heightened vulnerability to suicidal ideation.
A particularly distressing dimension uncovered by the researchers relates to the experiences of autistic individuals seeking professional mental health support. Numerous participants reported being misunderstood, disbelieved, and invalidated by healthcare professionals—a phenomenon that not only obstructed their path to effective treatment but also compounded feelings of hopelessness and alienation. These barriers to accessing empathetic, competent care were strongly linked to elevated suicide attempt rates, especially among autistic women and gender minorities, highlighting the necessity for specialized training and systemic reform within mental health services.
Diagnostic pathways and timelines emerged as another critical factor influencing mental health outcomes. The study detailed how many autistic individuals were overlooked during childhood diagnoses, leaving them with prolonged periods of uncertainty, confusion, and isolation during formative years. Compounding this issue, participants cited excessively long waiting lists for assessments and a lack of structured post-diagnostic support as contributing factors to persistent feelings of brokenness and despair, critical drivers of suicidal thoughts. This bottleneck in timely diagnosis and follow-up care compounds the risk of psychological crises over the lifespan.
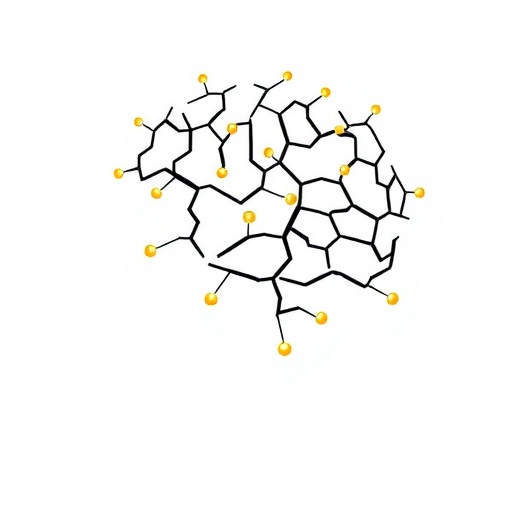
The charity Autism Action—a key instigator of the research—has framed these findings within the context of systemic “cracks” in UK healthcare and social care systems. These cracks represent not merely bureaucratic delays but causal levers with real, life-threatening repercussions for autistic individuals. The notion of “devastating delays” in autism assessments resonates deeply within the community and presents a striking call to policymakers. Autism Action further highlights the plight of both diagnosed and undiagnosed autistic people who find themselves bereft of meaningful support, a deprivation that intensifies vulnerability to mental health crises even further.
Dr. Moseley succinctly encapsulated the crux of this public health emergency: suicide in autistic people must be understood as a systemic issue, embedded within structural inequalities and inadequate access to education, employment, and healthcare services. These systemic failings not only amplify individual psychological risk factors but also generate an environment where many autistic people are effectively falling through the cracks. This framework compels a shift from individualized blame or stigma toward a recognition of widespread institutional responsibility.
The researchers urge urgent governmental intervention to rectify this crisis, recommending that reducing waiting times for autism assessments and expanding post-diagnostic support be prioritized as foundational steps. Moreover, augmenting the capacity and competencies of health and social care professionals to understand and cater to the unique needs of autistic individuals is vital. Without such measures, the status quo threatens to perpetuate suffering and increased mortality rates within this population.
Tom Purser, Chief Executive Officer of Autism Action, articulated the wider societal imperative reinforced by this study: government action is essential to create conditions wherein autistic people can enjoy dignified, meaningful lives, free from undue psychological distress and social marginalization. The scale and depth of insights provided by this research form a critical evidence base that Autism Action plans to leverage in advocacy efforts, pressing for systemic changes that can transform lives and stem the tide of suicide in autistic communities.
This pivotal research not only spotlights the urgent need for reform in healthcare and social service systems but also challenges prevailing narratives around autism by foregrounding the interplay between systemic inequities and mental health outcomes. As governments, healthcare providers, and societies grapple with these findings, the hope is that targeted, evidence-based interventions can emerge to address these profound vulnerabilities and cultivate more inclusive, supportive environments.
The implications of this study extend beyond the UK, resonating across global contexts where autistic individuals face similar structural barriers and societal stigmatization. It serves as both a diagnostic lens and a clarion call, urging a comprehensive reevaluation of how mental health, social care, and diagnostic services are conceived, funded, and delivered to disabled populations worldwide — particularly those living on the autism spectrum. The research thus represents a landmark contribution to understanding and mitigating the tragic mental health disparities confronting autistic individuals today.
Subject of Research: People
Article Title: “Cracks in the system” driving high suicide rates for autistic people
News Publication Date: 4-Sep-2025
Web References: DOI: 10.1177/25739581251371393
Keywords: Social sciences, Psychological science, Clinical psychology, Mental health, Psychiatry, Psychological stress, Psychotherapy, Cognitive psychology, Social research, Social surveys, Crisis intervention, Chronic stress, Stress management, Psychological assessment, Self help, Cognitive theory, Personality psychology, Emotions, Self perception, Social psychology