A medical anomaly so rare and insidious that it lurks silently beneath the veneer of apparent health has now been thrust into the spotlight. Researchers have documented an extraordinary case where sudden cardiac death was precipitated by an intussusception of a coronary artery—an event previously relegated to the realm of theoretical possibility rather than documented human pathology. This riveting case report, published in the International Journal of Legal Medicine, exposes uncharted territory in cardiovascular medicine and forensic pathology, shedding light on a mechanism of fatal cardiac arrest that challenges conventional diagnostic paradigms.
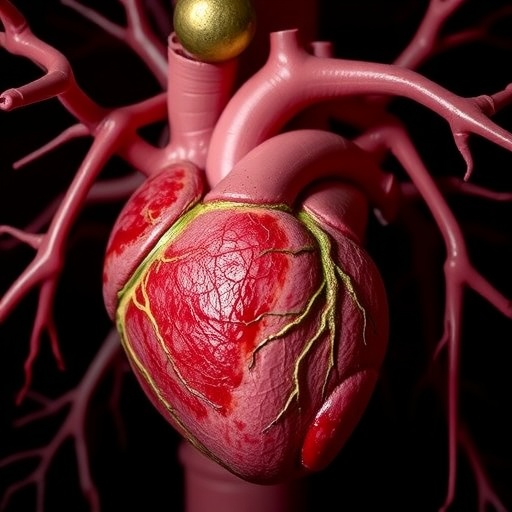
Intussusception, a phenomenon classically associated with the gastrointestinal tract, involves the telescoping of one segment of a hollow organ into an adjacent part, commonly invoking acute obstruction and ischemia. Its occurrence within a coronary artery vessel had been hitherto undocumented in human clinical cases, making this report a pioneering revelation. The coronary arteries, responsible for perfusing the myocardium, are critical conduits whose structural integrity is paramount for sustaining life. The unusual inward folding or invagination of a coronary artery segment in this instance led to catastrophic hemodynamic occlusion.
The clinical manifestation culminating in this fatal event was sudden cardiac death (SCD)—a tragic endpoint defined by an abrupt loss of cardiac function leading to death, often within minutes of symptom onset. SCD accounts for a significant proportion of mortality worldwide, predominantly linked to arrhythmias, myocardial infarction, or structural heart defects. However, the underlying causes can be cryptic in numerous cases, emphasizing the value of detailed post-mortem investigations such as this one.
The forensic autopsy unveiled intussusception as the causal lesion by demonstrating the unique morphological alterations within a coronary artery. The segment of the intussuscepted vessel created a mechanical obstruction akin to a physiological trap, severely restricting blood flow to critical myocardial territories. Microscopic examination reinforced the diagnosis by revealing disruption of the intimal layers and vascular wall architecture, hinting at the complex pathophysiological cascade that ensued prior to death.
What renders this case especially compelling is the rarity and diagnostic elusiveness of coronary artery intussusception. Unlike more familiar coronary pathologies such as atherosclerotic plaque rupture or embolism, intussusception lacks hallmark clinical signs and is invisible to conventional imaging techniques employed ante-mortem. The absence of warning symptoms, coupled with sudden occlusion, underscores this entity as a stealthy perpetrator in sudden cardiac fatalities.
The etiology behind the spontaneous intussusception remains speculative but intriguing hypotheses propose localized vessel wall weakness or aberrant contractile forces as contributing factors. Autoimmune or inflammatory processes could render the vascular layers susceptible to delamination, paving the way for telescoping under normal hemodynamic stress. Alternatively, congenital structural variants might predispose individuals to such vascular vulnerabilities.
Understanding these mechanisms not only expands the scientific comprehension of coronary artery diseases but also beckons a paradigm shift in how unexplained sudden cardiac deaths are approached. It challenges forensic pathologists and clinicians to consider uncommon vascular anomalies during autopsy and clinical evaluation, potentially refining protocols and preventative strategies.
The implications span beyond academic fascination; recognizing coronary intussusception can influence medico-legal outcomes and guide family counseling concerning inheritable risks. Genetic investigations alongside detailed histopathological scrutiny could pave the way for identifying at-risk individuals through innovative biomarkers or imaging modalities yet to be developed.
This case report also prompts a reexamination of current cardiovascular imaging technologies. Conventional angiography or computed tomography may not capture subtle intramural vascular distortions characteristic of intussusception. Future advancements like high-resolution intravascular ultrasound or optical coherence tomography might prove indispensable in detecting such elusive vascular phenomena.
Critically, this discovery sparks curiosity regarding potential therapeutic interventions. If identified preemptively, surgical correction or endovascular approaches might prevent catastrophic myocardial ischemia. However, the rarity and unpredictable nature of intussusception pose formidable challenges to the formulation of clinical guidelines.
From an investigative standpoint, the interdisciplinary collaboration between forensic medicine and cardiology was pivotal in unraveling this case. Such synergy exemplifies the importance of diverse expertise converging to decode perplexing medical mysteries, enhancing the collective arsenal against sudden cardiac deaths.
The broader medical community stands to gain immensely from heightened awareness of coronary artery intussusception. Educating clinicians, pathologists, and radiologists about this rare entity could incite more meticulous evaluations and reporting of similar cases globally. A growing database can yield epidemiological insights and inform future research trajectories.
Ultimately, this seminal case report is a clarion call to deepen investigative resolve in cases of sudden cardiac death where common etiologies fall short. It epitomizes the ceaseless quest for knowledge in medicine—unveiling hidden pathologies that lurk beneath the surface, forever reshaping our understanding of human health and disease.
Subject of Research: Sudden cardiac death caused by coronary artery intussusception
Article Title: Sudden cardiac death due to intussusception of a coronary artery: a case report
Article References:
Attico, F., Di Paola, F., De Nadai, M. et al. Sudden cardiac death due to intussusception of a coronary artery: a case report. Int J Legal Med (2025). https://doi.org/10.1007/s00414-025-03632-w
Image Credits: AI Generated